Le Infezioni in Medicina, n. 2, 157-167, 2024
doi: 10.53854/liim-3202-5
REVIEWS
Addressing the Dengue fever challenges in Nigeria: A narrative review and recommendations for control
Ridwan Olamilekan Adesola1, Favour Akinfemi Ajibade1, Ibrahim Idris2, Godfred Yawson Scott3, Mahmud Ibrahim Agaie4
1Department of Veterinary Medicine, Faculty of Veterinary Medicine, University of Ibadan, Ibadan, Nigeria;
2Faculty of Veterinary Medicine, Usmanu Dafodiyo University, Sokoto, Nigeria;
3Department of Medical Diagnostics, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana;
4School of Health Sciences, Department of Medical Laboratory Science, Biaka University Institute of Buea, Cameroon
Article received 16 February 2024, accepted 18 April 2024
Corresponding author
Ibrahim Idris
E-mail: ibrahimvet095@gmail.com
SummaRY
Dengue fever is a mosquito-borne viral infection that continues to pose a significant public health threat globally, including Nigeria. Here, we provided a review of dengue fever outbreaks in Nigeria from 1972 to 2023, examining the epidemiology, prevention strategies, challenges faced in combating the disease, and recommendations to mitigate its spread and transmission. We utilized scholarly databases such as PubMed and Google Scholar in writing this paper. The search keywords like, “dengue fever”, “break-bone fever”, “dengue fever virus” “outbreak”, “Nigeria”, “prevalence”, and “epidemiology”, were used to get appropriate published articles about the subject areas. Over the past five decades, Nigeria has experienced intermittent outbreaks of dengue fever, with varying degrees of severity and geographic distribution. Factors such as urbanization, climate change, and inadequate healthcare infrastructure have contributed to the resurgence and spread of the disease in the country. Despite efforts to control dengue transmission through vector control measures and public health interventions, challenges persist, including limited surveillance capacity, diagnostic delays, and gaps in vector control strategies. The emergence of new dengue virus serotypes and the potential for co-circulation with other arboviruses further complicate control efforts. This review highlights the importance of strengthening surveillance systems, enhancing vector control measures, improving diagnostic capabilities, and increasing public awareness to effectively mitigate the burden of dengue fever in Nigeria. Collaboration between government agencies, healthcare providers, researchers, and international partners is crucial in addressing the growing threat of dengue fever and reducing its impact on public health in Nigeria.
Keywords: Dengue fever, Nigeria, outbreaks, epidemiology, surveillance, vector control, public health.
BACKGROUND
Dengue fever (break-bone fever) is the most widespread disease caused by the dengue fever virus (DENV). DENV is carried by infected mosquitoes, especially Aedes species [1, 2]. DENV has four serotypes (1-4) with 62-67% sequence homology [3-5]. DENV genotypic classification was based on the patient’s immune responses to dengue fever [6]. Homologous DENV serotypes confer protection against secondary infection, but heterogenous serotypes confer transient protection [7].
According to the World Health Organization, dengue fever is endemic in more than 100 countries, with most incidents occurring in the Americas, Southeast Asia, and the Western Pacific [8]. The earliest known cases of dengue fever in Africa were recorded in Zanzibar, Tanzania, in 1823 and 1870 [5]. Later, in the early 1900s, unsubstantiated outbreaks of dengue fever were reported in several other African nations [6]. More than 20 laboratory-confirmed dengue fever epidemics were recorded in more than 20 African countries between 1960 and 2017, despite many outbreaks being never formally reported [6, 7].
Dengue fever is endemic in almost every state in Nigeria and is among the primary causes of feverish diseases that are misdiagnosed [8]. Dengue fever is distributed in both urban and rural regions, while reports of cases were historically more common in urban areas [9]. Nigeria has inadequate surveillance for dengue fever because the virus is not a public health priority, there is a lack of public awareness of it, and healthcare professionals do not fully understand its clinical presentation, as evidenced by the misdiagnosis and underdiagnosis of the viral infection in many unclassified febrile illnesses [10]. Nigeria’s dengue disease burden may be significantly underestimated [11]. A country is considered hyperendemic for dengue if all four serotypes are circulating concurrently [12].
The primary approaches for preventing and managing DENV transmission are case detection, management, and vector control [12]. Making informed decisions about the most effective use of current and emerging preventive and control methods in Nigeria requires up-to-date knowledge about the burden, incidence, and geographic distribution of dengue fever. To address this need, we provided an updated review of dengue fever outbreaks in Nigeria from 1972 to 2023, examining the epidemiology, prevention strategies, challenges faced in combating the disease, and recommendations to mitigate its spread and transmission.
METHODS
In writing this review, we utilized scholarly databases such as PubMed and Google Scholar. The search keywords “dengue fever”, “break-bone fever”, “dengue fever virus” “outbreak”, “Nigeria”, “prevalence”, and “epidemiology”, were used to get appropriate published articles about the subject areas. This review includes data exclusively from studies conducted in Nigeria that focus on the epidemiology or clinical aspects of dengue fever, while excluding studies on other topics.
RESULTS AND DISCUSSIONS
Dengue fever: past and present
Dengue fever has a long history, with the earliest documented case of a disease resembling it noted in a Chinese medical encyclopaedia dating back to 992 AD [13]. The disease was referred to as ‘water poison’ and was associated with flying insects [14]. The primary vector, Aedes aegypti mosquitoes, which are central to the emergence of the disease as a public health problem, spread out of Africa in the 15th to 19th centuries, partly due to increased globalization secondary to the slave trade, and is widely distributed through the tropical and subtropical regions of the world [15]. Although there have been descriptions of dengue fever epidemics since the 17th century, the earliest credible records of such outbreaks were from 1779 and 1780, when an epidemic struck Asia, Africa, and North America. From that time, epidemics were infrequent until the 1940s [16]. Transmission by Aedes mosquitos was confirmed in 1906, and dengue fever was the second disease (after yellow fever) to be shown to be caused by a virus in 1907 [17].
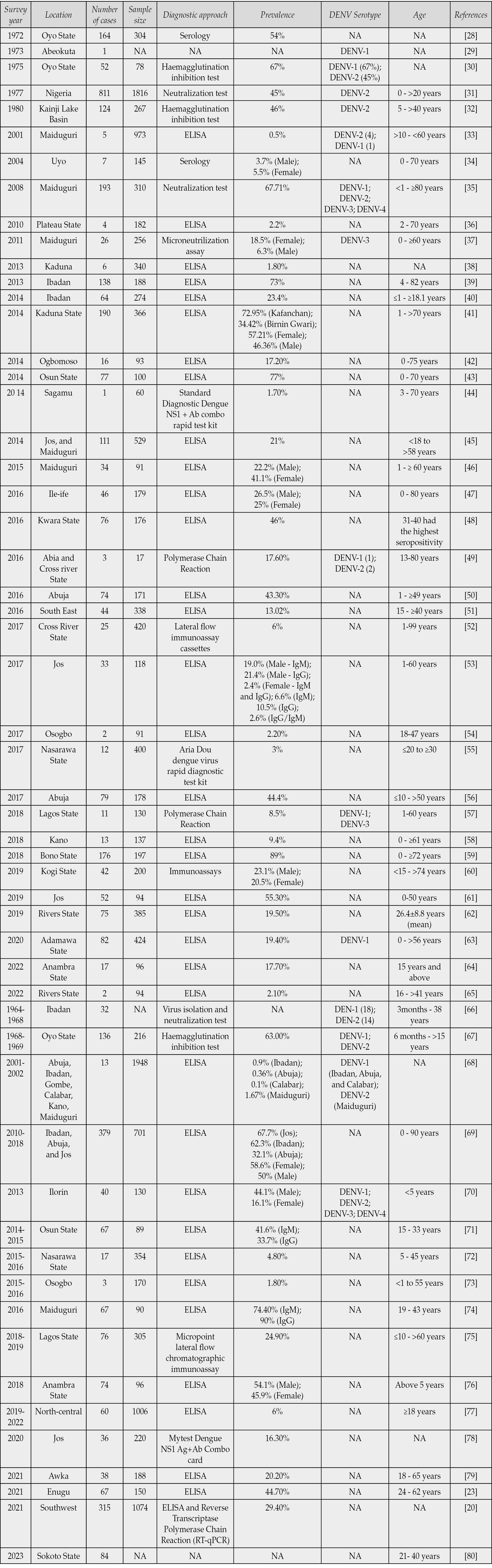
Dengue virus was first described in Nigeria in the 1960s in Ibadan [18]. Although there were numerous reports of isolated outbreaks in Nigeria after 1960 (Table 1), many of the outbreaks were likely unreported, unidentified, or neglected due to a lack of diagnostic tools and uninformed health professionals in medical facilities about the disease [19]. Additionally, most cases of dengue fever are misdiagnosed as malaria or typhoid fever in most healthcare facilities [20]. In Nigeria, dengue fever is endemic in almost all states and may be the leading cause of unclassified febrile illness [21]. Dengue fever has a different prevalence in urban and rural areas and has been reported predominantly in urban areas rather than rural areas [21].
Table 1 - Summary of dengue fever cases recorded in Nigeria from 1972 to 2023.
According to Emeribe et al. [21], surveillance of dengue fever in Nigeria is subpar [21]. There is a lack of public awareness of the virus and a lack of understanding by medical professionals, resulting in the misdiagnosis and underdiagnosis of the viral infection evident by the many categorized febrile illnesses [22]. However, the importance and knowledge of the disease are fast-growing. Recent IgM seroprevalence surveys conducted in Enugu and Lagos showed that 44.70% and 24.90% of participants, respectively, were seropositive for anti-dengue antibodies [23, 24]. Additionally, dengue NS1, IgM, and IgG seroprevalence surveys among febrile Nigerian patients in rural areas of Southwestern Nigeria who presented with malaria and typhoid fevers showed a prevalence of 29.4% (315/1074) [20].
These high prevalence rates of both symptomatic dengue virus infections and dengue IgM antibodies suggest that dengue may be endemic and that, frontline healthcare personnel may have missed numerous infections. There is evidence of high vector density in Nigeria’s densely populated cities, with a high density of the Aedes aegypti mosquito that transmits dengue, yellow fever (YFV), and chikungunya, and the same applies to the Anopheles mosquito that transmits malaria, masking the diagnosis of dengue fever [25, 26].
The recent outbreak of dengue fever reported by the Nigeria Centre for Disease Control and Prevention on December 16th, 2023, in Sokoto, Nigeria, further highlights the growing significance of the disease [27]. So far, there have been 13 confirmed cases in the state. These findings suggest that dengue fever is a growing public health problem in Nigeria, the extent of which needs to be more clearly defined, with a dire need for an effective response to prevent and control the disease to safeguard public health.
In Table 1 are reported various studies that have detected dengue fever virus in different geographical locations of Nigeria from the past (1972) to the present (2023). Plateau State has been shown to have the highest number of cases of dengue fever in Nigeria. Also, all four serotypes of dengue fever virus (DENV-1 to -4) available in different parts of Nigeria have been shown in Table 1. There have been similarities and differences between the past and present outbreaks of dengue fever in Nigeria. Enzyme Linked Immunosorbent Assay (ELISA) has been the most frequently used diagnostic method for the detection of dengue fever. This is in support of our claim for the need for molecular diagnostic tools in Nigeria. The methods of control of dengue fever are the same during the outbreaks. Vector control and supportive therapy are the only methods used to prevent and control dengue in Nigeria. Furthermore, most of the outbreaks have been attributed to adult individuals rather than children. These might be as a result of higher exposure of adults to mosquito bites than children [81].
CHALLENGES ASSOCIATED WITH INCREASING CASES OF DENGUE FEVER IN NIGERIA
Exhaustion of medical facilities: In Nigeria, dengue fever epidemics frequently strain existing limited medical facilities. There is a rise in hospital admissions during significant outbreaks of dengue fever. As a result, there are several challenges facing the country’s health services, including a lack of hospital beds, drugs, hospital supplies, and laboratory reagents and equipment.
Limited educational and sensitization program about dengue fever: Education prospects in Nigeria are dire. The Federal Government claims a countrywide literacy rate of 69%, however this number conceals substantial regional variations. Yobe, with 7.23% of the population, had the lowest literacy rate in 2017, followed by Zamfara (19.16%), Katsina (10.36%), and Sokoto (15.01%), according to a National Bureau of Statistics report [82]. The Nigerian health authorities have reported the highest outbreaks of dengue fever in Sokoto State between 2016 and 2019 [83]. The lack of comprehensive education to recognize the clinical presentation and symptoms of dengue fever, coupled with the misdiagnosis of the disease as malaria by healthcare professionals, could contribute to this situation. Implementing an extensive national campaign and sensitization program is imperative for the current management and future disease eradication efforts.
Mosquito breeding site: One of the significant challenges contributing to the increasing cases of dengue fever in Nigeria is the proliferation of mosquito breeding sites. The conducive environment for mosquito breeding, such as stagnant water in containers, discarded tires, and other receptacles, provides ample opportunities for Aedes mosquitoes, the primary vectors of dengue fever, to reproduce rapidly. Inadequate sanitation infrastructure, urbanization, and poor waste management techniques all contribute to the problem by giving mosquitoes more places to breed.
COVID-19 pandemic: The occurrence of COVID-19 in Nigeria affected the healthcare system severely. The attention of many healthcare practitioners was on the eradication and control of COVID-19. Most of the other febrile infectious diseases such as dengue fever were neglected which has resulted in the increasing alarming rate of dengue in Nigeria.
Lack of DENV blood screening facilities: Although dengue spread through transfusion is uncommon, Nigeria does not have a licensed donor screening test for DENV. As a result, during epidemics, many blood donations cannot be collected. Strict donor selection protects blood-transmitted DENV, but it is labor-intensive, expensive, jeopardizes supply sufficiency, and might not be feasible.
Recommendation to mitigate the current and future outbreaks
- In Nigeria, there is a need for more thorough attention and dedication to improve the detection of febrile illnesses. Given that malaria, yellow fever, chikungunya, and dengue have clinically similar causes of fever, laboratory surveillance of dengue is essential for improving dengue detection and confirmation. Offering NS1 dipstick dengue testing at the primary healthcare level could be a brave move in the right direction. In addition to having a reasonable sensitivity and specificity profile and quick findings, the NS1 dipstick test is comparatively simple to perform.
- The Federal Ministry of Health in Nigeria should prioritize funding for nationwide dengue surveys to assess the prevalence and distribution of different dengue serotypes across the country. These surveys will provide crucial data to inform public health strategies and interventions aimed at controlling the spread of dengue fever. Additionally, efforts should be made to incorporate dengue as a recognized disease in medical school curricula. By educating young medical practitioners about dengue fever symptoms, diagnosis, and treatment, future healthcare professionals will be better equipped to identify and manage cases of dengue fever effectively. This proactive approach will enhance the healthcare system’s capacity to respond to dengue outbreaks and reduce the burden of the disease on affected communities in Nigeria. To identify the dengue serotypes and their vectors throughout the nation, concurrent virus identification assays, vector surveillance, and nationwide dengue surveys should all be conducted at the same time. It is necessary to put up a comprehensive and integrated dengue disease monitoring system, connect it to the national health information system, and keep an eye on several key indicators. Developing outbreak preparedness with the appropriate agencies ought to be a top focus.
- Source reduction is important and should involve environmental modification techniques such as covering or lidding water containers and, if feasible, getting rid of them. Although it has been documented that Aedes aegypti and Aedes albopictus are resistant to pyrethroids and organophosphates (temephos), the use of these insecticides is advantageous. The population of disease-carrying vectors has been demonstrated to be reduced by 95% with the use of genetically modified (GM) mosquitoes [84]. The two ways in which genetically modified mosquitoes function are through “population replacement” which replaces a mosquito population with one incapable of spreading infections. The mosquito can become infected with Wolbachia, a bacterial symbiont that inhibits the mosquito’s capacity to spread other infections. The second strategy, known as “population suppression”, can be carried out by producing sterile male mosquitoes by the Sterile Insect Technique (SIT), which will eventually cause the population of mosquitoes to decline. Leveraging effective vector management strategies is a logical and impactful approach, particularly in Nigeria where challenges such as inadequate sewage and water infrastructure, rapid urbanization, and unplanned development contribute to favourable conditions for mosquito breeding. By intensifying efforts in vector control, Nigeria can address the root causes of mosquito proliferation and subsequently reduce the transmission of diseases like dengue fever in Nigeria. Achieving success in combating dengue fever hinges on strengthening the capabilities of frontline healthcare professionals and elevating dengue as a priority in fever management in Nigeria. Advocating for robust health worker training programs and the implementation of clinical algorithms tailored to dengue diagnosis and management is essential. By equipping healthcare providers with the necessary knowledge and tools, we can enhance the timely and accurate identification of dengue cases across Nigeria. Moreover, it is imperative to involve laboratory scientists and entomologists in capacity-building initiatives to bolster vector identification and management efforts. By fostering collaboration among multidisciplinary teams, we can advance our collective ability to diagnose, treat, and prevent dengue fever effectively, ultimately reducing its burden on the population. The aim of infectious disease prevention is the creation of a vaccine that works. The goal of the Dengue Vaccine Initiative is to expedite the creation of a dengue vaccine that is both safe and effective, protecting against all serotypes. In addition to additional possibilities in pre-clinical testing, five vaccine candidates are presently undergoing human testing. The vaccine candidate from Sanofi Pasteur has demonstrated partial (~30-60%) protection against dengue infection. The investigation of the intricate relationships between dengue and the human immune system has been impeded by the absence of suitable laboratory animal models to study dengue infection [9]. Further research in this field may help produce more potent vaccines.
CONCLUSION
In Nigeria, dengue cases are underreported due to inadequate surveillance and misdiagnoses. Determining the extent of dengue fever in the nation and gathering information for health planning, which includes budgeting for diagnosis, treatment, and control, would be made easier with the help of accurate case reporting. To help with timely and accurate identification of the causative agent and control of dengue fever epidemics, the federal government should prioritize capacity building for monitoring and emergency response systems, laboratory diagnosis, and infrastructure. Currently, the nation’s laboratory diagnostic capabilities for dengue are limited to a small number of setups and personnel. It is necessary to fortify these labs, construct new ones, and stock them with cutting-edge technology including test reagents, contemporary equipment, and trained personnel.
Authors’ contribution
All authors contributed equally to writing the manuscript.
Conflict of interest
The authors declare that they have no competing interests.
Ethical clearance
Not Available.
Funding
No funding.
REFERENCES
[1] Powell JR. Mosquito-borne human viral diseases: why Aedes aegypti? Am J Trop Med Hyg. 2018; 98(6): 1563.
[2] Akinsulie OC, Adesola RO, Aliyu VA, Oladapo IP, Hamzat A. Epidemiology and transmission dynamics of viral encephalitides in West Africa. Infect Dis Rep. 2023; 15(5): 504-517.
[3] Onoja BA, Maiga M, Adesola RO, Adamu AM, Adegboye OA. Changing ecotypes of dengue virus 2 serotype in Nigeria and the emergence of cosmopolitan and Asian i lineages, 1966-2019. Vaccines (Basel). 2023; 11(3): 547.
[4] de Bruycker-Nogueira F, Nogueira RM, da Costa Faria NR, et al. Insights of the genetic diversity of DENV-1 detected in Brazil in 25 years: Analysis of the envelope domain III allows lineages characterization. Infect Genet Evol. 2015; 34: 126-136.
[5] Tamura T, Zhang J, Madan V, et al. Generation and characterization of genetically and antigenically diverse infectious clones of dengue virus serotypes 1-4. Emerg Microbes Infect. 2022; 11(1): 227-239.
[6] Soo KM, Khalid B, Ching SM, Chee HY. Meta-analysis of dengue severity during infection by different dengue virus serotypes in primary and secondary infections. PloS one. 2016; 11(5): e0154760.
[7] Izmirly AM, Alturki SO, Alturki SO, Connors J, Haddad EK. Challenges in dengue vaccines development: pre-existing infections and cross-reactivity. Front Immunol. 2020; 11: 1055.
[8] World Health Organization (WHO). Dengue - the Region of the Americas. 2023. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON475#:~:text=The%20disease%20is%20now%20endemic,of%20the%20global%20disease%20burden. [Accessed on 10th February, 2024].
[9] Vong S, Khieu V, Glass O, et al. Dengue incidence in urban and rural Cambodia: results from population-based active fever surveillance, 2006-2008. PLoS Negl Trop Dis. 2010; 4(11): e903.
[10] Nasir IA, Agbede OO, Dangana A, Baba M, Haruna AS. Dengue virus non-structural Protein-1 expression and associated risk factors among febrile Patients attending University of Abuja Teaching Hospital, Nigeria. Virus Res. 2017; 230: 7-12.
[11] Ayukekbong JA, Oyero OG, Nnukwu SE, Mesumbe HN, Fobisong CN. Value of routine dengue diagnosis in endemic countries. World J Virol. 2017; 6(1): 9-16.
[12] Sirisena PDN, Mahilkar S, Sharma C, Jain J, Sunil S. Concurrent dengue infections: Epidemiology & clinical implications. Indian J Med Res. 2021; 154(5): 669-679.
[13] Gubler DJ. Dengue/dengue haemorrhagic fever: history and current status. Novartis Found Symp. 2006; 277: 3-16.
[14] Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998; 11(3): 480-496.
[15] Simmons CP, Farrar JJ, Nguyen vV, Wills B. Dengue. N Engl J Med. 2012; 366(15): 1423-1432.
[16] Henchal EA, Putnak JR. The dengue viruses. Clin Microbiol Rev. 1990; 3(4): 376-96.
[17] Wilder-Smith A, Gubler DJ. Geographic expansion of dengue: the impact of international travel. Med Clin North Am. 2008; 92(6): 1377-1390.
[18] World Health Organization (WHO). Global strategy for dengue prevention and control 2012-2020. 2012. Available at: https://www.who.int/publications-detail-redirect/9789241504034 [Accessed on 12th February, 2024].
[19] Baba MM, Talle M. The effect of climate on dengue virus infections in Nigeria. West Afr J Med. 2022; 39(10): 1104-1107.
[20] Okoror LE, Bankefa EO, Ukhureigbe OM, Ajayi EO, Ojo SK, Ogeneh B. Misdiagnosis of dengue fever and co-infection with malaria and typhoid fevers in rural areas in Southwest Nigeria. Res Squar. 2021.
[21] Emeribe AU, Abdullahi IN, Isong IK, et al. Dengue virus is hyperendemic in Nigeria from 2009 to 2020: a contemporary systematic review. Infect Chemother. 2021; 53(2): 284.
[22] Amarasinghe A, Kuritsky JN, Letson GW, Margolis HS. Dengue virus infection in Africa. Emerg Microbes Infect. 2011; 17(8): 1349.
[23] Esimone CO, Abone HO, Ezea MC, et al. Dengue in co-infection with Hepatitis B virus in Enugu, Eastern Nigeria: Seroprevalence, impacts, and risk of increasing transmission. UNIZIK. 2021.
[24] Mohammed A, Odegbemi O, Igwe C, Hussain N, Abaye B, Adekanye U. Prevalence and determinants of dengue virus immunoglobulin among febrile patients attending naval medical Centre Victoria Island, Lagos State. Glob Bios. 2021; 3(1).
[25] Otu A, Ebenso B, Etokidem A, Chukwuekezie O. Dengue fever-an update review and implications for Nigeria, and similar countries. Afr Health Sci. 2019; 19(2): 2000-2007.
[26] Baba M, Logue CH, Oderinde B, et al. Evidence of arbovirus co-infection in suspected febrile malaria and typhoid patients in Nigeria. J Infect Dev Ctries. 2013; 7(01): 051-059.
[27] Nigeria Centre for Disease Control and Prevention (NCDC). Available at: https://ncdc.gov.ng/news/506/ncdc-on-alert-following-the-confirmation-of-the-dengue-fever-outbreak-in-sokoto-state.#:~:text=The%20Nigeria%20Centre%20for%20Disease,been%20reported%20in%20the%20state [Accessed on 26th December, 2023]
[28] Fagbami A. Human arthropod-borne virus infections in Nigeria. Serological and virological investigations and Shaki, Oyo State. J Hyg Epidemiol Microbiol Immunol. 1978; 22(2): 184-189.
[29] Fagbami AH, Tomori O, Fabiyi A. Clinical and virological observations during an outbreak of dengue and dengue-like illness at Abeokuta, Nigeria. Nig Med J. 1977; 7: 380-383.
[30] Fagbami A. Epidemiological investigations on arbovirus infections at Igbo-Ora, Nigeria. Trop Geogr Med. 1977; 29(2): 187-191.
[31] Fagbami AH, Monath TP, Fabiyi A. Dengue virus infections in Nigeria: a survey for antibodies in monkeys and humans. Trans R Soc Trop Med Hyg. 1977; 71(1): 60-65.
[32] Adekolu-John EO, Fagbami AH. Arthropod-borne virus antibodies in sera of residents of Kainji Lake Basin, Nigeria 1980. Trans R Soc Trop Med Hyg. 1983; 77(2): 149-151.
[33] Baba MM, Talle M. The effect of climate on dengue virus infections in Nigeria. New York Sci Jour. 2011; 4(1): 28-33.
[34] Moses A, Atting I, Inyang O. Evidence of overlapping infections of dengue, malaria and typhoid in febrile patients attending a tertiary health facility in Uyo, South-South Nigeria. Brit J Med Res. 2016; 17(3): 1-9.
[35] Baba M, Logue CH, Oderinde B, et al. Evidence of arbovirus co-infection in suspected febrile malaria and typhoid patients in Nigeria. J Infect Dev Ctries. 2013; 7(01): 51-59.
[36] Dawurung JS, Baba MM, Stephen G, Jonas SC, Bukbuk DN, Dawurung CJ. Serological evidence of acute dengue virus infection among febrile patients attending Plateau State Specialist Hospital Jos, Nigeria. UniJos. 2010; 2(6): 71-76.
[37] Idris AN, Baba MM, Thairu Y, Bamidele O. Sero-prevalence of dengue type-3 Virus among patients with febrile illnesses attending a tertiary hospital in Maiduguri, Nigeria. Int J Med Med Sci. 2013; 5(12): 560-563.
[38] Idoko M, Ado S, Umoh V. Prevalence of dengue virus and malaria in patients with febrile complaints in Kaduna Metropolis, Nigeria. Brit J Med and Med Res. 2015; 8(1): 343-347.
[39] Oyero OG, Ayukekbong JA. High dengue NS1 antigenemia in febrile patients in Ibadan, Nigeria. Virus Res. 2014; 191: 59-61.
[40] Onoja AB, Adeniji JA, Olaleye OD. High rate of unrecognized dengue virus infection in parts of the rainforest region of Nigeria. Acta Tropica. 2016; 160: 39-43.
[41] Bello OA, Aminu M, Jatau ED. Seroprevalence of IgM antibodies to dengue fever virus among patients presenting with symptoms of fever in some hospitals in Kaduna State Nigeria. Int J Sci Res. 2016; 5(3): 1255-1259.
[42] Adekolu-John EO, Fagbami AH. Arthropod-borne virus antibodies in sera of residents of Kainji Lake Basin, Nigeria 1980. Trans R Soc Trop Med Hyg. 1983; 77(2): 149-151.
[43] Adeleke MA, Muhibi MA, Ajayi EI, et al. Dengue virus specific Immunoglobulin G antibodies among patients with febrile conditions in Osogbo, Southwestern Nigeria. Trop Biomed. 2016; 33(1): 1-7.
[44] Ayorinde AF, Oyeyiga AM, Nosegbe NO, Folarin OA. A survey of malaria and some arboviral infections among suspected febrile patients visiting a health centre in Simawa, Ogun State, Nigeria. J Infect Public Health. 2016; 9(1): 52-59.
[45] Onyedibe K. A cross sectional study of dengue virus infection in febrile patients presumptively diagnosed of malaria in Maiduguri and Jos plateau, Nigeria. Malawi Med J. 2018; 30(4): 276-282.
[46] Hamisu TM, El-Yuguda AD, Abubakar MB, et al. Prevalence of Dengue virus infection among febrile outpatients attending University of Maiduguri Teaching Hospital in Borno State, Nigeria. IOSR J Dent Med Sci. 2017; 16: 155-159.
[47] Adesina OA, Adeniji JA. Incidence of dengue virus infections in febrile episodes in Ile-Ife, Nigeria. Afr J Infect Dis. 2016; 10(1): 21-24.
[48] Kolawole OM, Seriki AA, Irekeola AA, Bello KE, Adeyemi OO. Dengue virus and malaria concurrent infection among febrile subjects within Ilorin metropolis, Nigeria. J Med Virol. 2017; 89(8): 1347-1353.
[9] Onoja AB, George UE, Gadzama IS. Co-circulation of dengue virus 1 and 2 several years after single serotype detection in Cross River State, Nigeria. Sok J Vet Sci. 2020; 18(3): 167-170.
[50] Nasir IA, Agbede OO, Dangana A, Baba M, Haruna AS. Dengue virus non-structural Protein-1 expression and associated risk factors among febrile Patients attending University of Abuja Teaching Hospital, Nigeria. Virus Res. 2017; 230: 7-12.
[51] Osarumwense OI, Nkechukwu IM, Favour EN, et al. The prevalence of Dengue virus and malaria co-infection among HIV-infected patients within South Eastern Nigeria. Adv Infect Dis. 2022; 12(1): 106-117.
[52] Otu AA, Udoh UA, Ita OI, Hicks JP, Egbe WO, Walley J. A cross-sectional survey on the seroprevalence of dengue fever in febrile patients attending health facilities in Cross River State, Nigeria. PLoS One. 2019; 14(4): e0215143.
[53] Kingsley UB, Tabitha VS, Lohya N, Joseph AO. Dengue virus antibodies in patients presenting with pyrexia attending Jos University Teaching Hospital, Jos, Nigeria. Saudi J Pathol Microbiol. 2018; 3: 47-55.
[54] Muhibi MA, Adeleke MA, Shittu BT, Jeremiah ZA. Dengue Virus Infection among Voluntary Blood Donors in Osogbo, Southwestern Nigeria. Am J Biomed Sci. 2017; 9(3): 113-118.
[55] Suchi NK, Mohammed HI, Ademola AO, Rinmecit PG. Parallel and concurrent infection of Dengue virus and Plasmodium falciparum among patients with febrile illnesses attending Bingham University Health Centre, Karu, Nigeria. Int J Trop Dis & Heal. 2020; 41(12): 45-51.
[56] Mustapha JO, Emeribe AU, Nasir IA. Survey of malaria and anti-dengue virus IgG among febrile HIV-infected patients attending a tertiary hospital in Abuja, Nigeria. HIV/AIDS-Res. 2017; 9: 145-151.
[57] Ayolabi CI, Olusola BA, Ibemgbo SA, Okonkwo GO. Detection of Dengue viruses among febrile patients in Lagos, Nigeria and phylogenetics of circulating Dengue serotypes in Africa. Infect Genet Evol. 2019; 75: 103947.
[58] Nas FS, Ali M, Mu’azu L, Abdallah MS. Seroprevalence of Dengue Fever among Febrile Patients Attending Kura General Hospital Kano, Nigeria? Mathews J Immunl Allergy. 2020; 4(1): 10.
[59] Oderinde BS, Mora-Cárdenas E, Carletti T, Baba MM, Marcello A. Prevalence of locally undetected acute infections of Flaviviruses in North-Eastern Nigeria. Virus Res. 2020; 286: 198060.
[60] Omatola CA, Onoja AB, Moses E, Mahmud M, Mofolorunsho CK. Dengue in parts of the Guinea Savannah region of Nigeria and the risk of increased transmission. Int Health. 2021; 13(3): 248-252.
[61] Miri NF, Mawak JD, Chukwu CO, Chuwang NJ, Acheng SY, Ezekiel T. Detection of IgM and IgG Dengue antibodies in febrile patients suspected of malaria attending health center in Jos, Nigeria. Ann Med Lab Sci. 2021; 1(1): 27-35.
[62] Harcourt IP. Seroprevalence of dengue imunoglobulins and awareness of dengue fever among healthy blood donors in Port Harcourt, Nigeria. Int J Infect Dis. 2021; 30(5).
[63] Tizhe DT, Kwaga JK, Nok Kia GS. Serological and molecular survey for dengue virus infection in suspected febrile patients in selected local government areas in Adamawa State, Nigeria. Vaccines. 2022; 10(9): 1407.
[64] Michael NI, Chimuanya UK, Mariagoretti CO, Onochie MP, Okechukwu CG. Detection of Dengue Virus IgM seropositivity and malaria co-infection among individuals resident on the banks of river Niger in Anambra State, Nigeria. Int J Trop Dis & Health. 2023; 44(7): 31-38.
[65] Okonko IO, Innocent-Adiele HC, Njoku OV, Eugene EA. First serological prevalence of dengue virus IgG antibody among pregnant women in Port Harcourt, Nigeria. Sci Afr. 2023; 22(2): 239-248.
[66] Carey DE, Causey OR, Reddy S, Cooke AR. Dengue viruses from febrile patients in Nigeria, 1964-68. The Lancet. 1971; 297(7690): 105-106.
[67] Fagbami A. Epidemiological investigations on arbovirus infections at Igbo-Ora, Nigeria. Trop Geog Med. 1977; 29(2): 187-91.
[68] Baba MM, Saron MF, Vorndam AV, Adeniji JA, Diop O, Olaleye D. Dengue virus infections in patients suspected of malaria/typhoid in Nigeria. J Am Sci. 2009; 5(5): 129-134.
[69] Ekong PS, Aworh MK, Grossi-Soyster EN, et al. A retrospective study of the seroprevalence of dengue virus and chikungunya virus exposures in Nigeria, 2010–2018. Pathogens. 2022; 11(7): 762.
[70] Adedayo F, Nioma I, Olanrewaju MB, Adeyinka A, Ebele A. Serological evidence of recent dengue virus infection among febrile children in a semi-arid zone. Am J of Infect Dis. 2013; 9(1): 7.
[71] Sule WF, Fadamitan TO, Lawal OA, Adebimpe WO, Opaleye OO, Oluwayelu DO. Probable primary and secondary dengue viral infections and associated host factors among university undergraduates in Osun State, Nigeria. Alex J Med. 2019; 55(1): 25-30.
[72] Abubakar AA, Fatima J, Colin BS, Ahmed SA, Adebola O. Seroprevalence and associated risk factors of Dengue virus among apparently healthy individuals in Karu Local Government Area, Nasarawa State, Nigeria. Ann Trop Med Pathol. 2022; 13(2): 86-91.
[73] Nassar SA, Olayiwola JO, Bakarey AS, Enyhowero SO. Investigations of dengue virus and Plasmodium falciparum among febrile patients receiving care at a tertiary health facility in Osogbo, south-west Nigeria. Nig J Parasitol. 2019; 40(1).
[74] Oyinloye SO, Wajiroko M, Lawan AM, Umar-Faruq A, Samuel-Bumba M, Yusuf S. Dengue virus infection in northeast Nigeria: case study of a squatters’ Camp. Int J Perceptions Pub Health. 2016; 1(1): 59-65.
[75] Mohammed A, Odegbemi O, Igwe C, Hussain N, Abaye B, Adekanye U. Prevalence and determinants of Dengue virus immunoglobulin among febrile patients attending naval medical centre Victoria Island, Lagos State. Glob Bios. 2021; 3(1).
[76] Chukwuma GO, Audu JS, Chukwuma OM, et al. Seroprevalence of dengue virus among children with febrile illness in Nnewi, Nigeria. J Med Res. 2018; 4(1): 24-30.
[77] Ogwuche J, Chang CA, Ige O, et al. Arbovirus surveillance in pregnant women in north-central Nigeria, 2019-2022. J Clin Virol. 2023; 169: 105616.
[78] Katnap RS, Dangari AM, Nkup JY, Nimzing L, Lar PM, Egah DZ. Prevalence of dengue virus infection and malaria parasitaemia in febrile patients in Jos South, Plateau State, Nigeria. Adv Micro Biotech Res J. 2020; 1(1): 14-19.
[79] Linda O, Chimere V, George OC. Determination of Dengue Virus IGM Seroprevalence, Malaria Parasitaemia and Some Haematological Parameters of HIV Infected Individuals in Awka, Nigeria. J Adv Microbiol. 2021; 21(12): 17-29.
[80] Tizhe DT, Dashe DF, Kwaga JK. Dengue fever in Nigeria: a mini review. EUREKA: Life Sci. 2023; (2): 63-70.
[81] Guglielmo F, Sanou A, Churcher T, Ferguson HM, Ranson H, Sherrard-Smith E. Quantifying individual variability in exposure risk to mosquito bites in the Cascades region, Burkina Faso. Malar J. 2021; 20(1): 44.
[82] Oradi O. Introduction: An Appraisal of Nigeria’s Implementation of the “Quality Education” Goal. ORADI. 2019.
[83] Mohammed Y, Obi IF, Aniaku EC, et al. An Outbreak of Arboviral Infection in a Region with Background Malaria Endemicity from Northwestern Nigeria: An Investigation Report. West Afr J Med. 2021; 38(10): 993-998.
[84] Finkel AM, Trump BD, Bowman D, Maynard A. A “solution-focused” comparative risk assessment of conventional and synthetic biology approaches to control mosquitoes carrying the dengue fever virus. Environment Systems and Decisions 2018; 38: 177-197.