Le Infezioni in Medicina, n. 2, 148-156, 2024
doi: 10.53854/liim-3202-4
REVIEWS
Cholera resurgence in Africa: assessing progress, challenges, and public health response towards the 2030 global elimination target
Blessing Olawunmi Amisu1, Olalekan John Okesanya2, Olaniyi Abideen Adigun3, Emery Manirambona4, Bonaventure Michael Ukoaka5, Okikiola Azeez Lawal6, Nimat Bola Idris7, Noah Olabode Olaleke8, Inibehe Ime Okon9, Jerico Bautista Ogaya10, Don Eliseo Lucero Prisno III11
1Department of Medical Laboratory Science, Uniosun Teaching Hospital, Osogbo, Osun state, Nigeria;
2Department of Public Health and Maritime Transport, University of Thessaly, Volos, Greece;
3Department of Medical Laboratory Science, University College Hospital, Ibadan, Nigeria;
4College of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda;
5Department of Internal Medicine, Asokoro District Hospital, Abuja, Nigeria;
6Department of Medical Laboratory Sciences, Kwara State University, Kwara State, Nigeria;
7Department of Public Health, Al-Hikmah University, Ilorin, Kwara State, Nigeria;
8Department of Medical Laboratory Science, Obafemi Awolowo University Teaching Hospitals Complex, Ile Ife, Osun State, Nigeria;
9Department of Neurosurgery, Hospital of the Babcock University, Ogun State, Nigeria;
10Department of Medical Technology, Far Eastern University, Manila, Philippines;
11Department of Global Health and Development, London School of Hygiene and Tropical Medicine, London, United Kingdom
Article received 12 February 2024, accepted 14 April 2024
Corresponding author
Okesanya Olalekan John
E-mail: okesanyaolalekanjohn@gmail.com
SummaRY
Global efforts to combat epidemic cholera outbreaks have witnessed tremendous feats over the decades. However, sporadic outbreaks in regions, particularly across African states, mask these advancements. This regressive trend is frequently fuelled by factors retarding efforts towards optimal environmental sanitation and personal hygiene, which include ingesting infected food, drinking contaminated waters, and engaging in unhealthy environmental practices such as indiscriminate waste and sewage disposal and poor toilet practices. The ongoing efforts to achieve the Global Taskforce on Cholera Control (GTFCC) targets of a 90% reduction in cases and deaths by 2030, even in the wake of continuous outbreaks across various African regions, as reported by the World Health Organization (WHO) face a significant threat. One such effort, among others, is the AFRICHOL project, an enhanced cholera surveillance consortium launched in Africa over a decade ago as part of the GTFCC at WHO to monitor and fast-track the GTFCC’s 2030 targets. It is tasked with supporting the implementation of research-based strategies for combating cholera in Africa. The prequalified oral cholera vaccines – Dukoral, Shanchol, and Euvichol – and those with recombinant DNA technology have also emerged as remarkable strides. In the face of this progress, challenges persist. Climate change, including extreme weather events and the lack of safe water, sanitation, and hygiene facilities, acts as a multiplier, amplifying existing challenges and hindering progress. Porous borders with inefficient disease surveillance networks among member states also facilitate the inter-territorial spread of the disease. Despite ongoing challenges, global targets are achievable provided strong institutional infrastructure and additional evidence-based public health initiatives are promulgated and enacted. The Global Roadmap to Ending Cholera Outbreaks by 2030 is a resourceful tool for advancing this fight and eradicating cholera.
Keywords: Cholera outbreak, water, sanitation, and hygiene (WASH), public health response, cholera vaccines, Africa.
INTRODUCTION
Cholera, a waterborne disease caused by the Vibrio cholerae bacterium, has reemerged in Africa, posing a renewed threat and public health challenge across the continent [1]. The cholera outbreak in Haiti in 2010 brought a previously ignored disease to the global limelight. This return has raised global health concerns, prompting the activation of existing disease surveillance networks to check for and manage impending adverse outcomes. The AFRICHOL project – a cholera surveillance network in Africa supported by the World Health Organization (WHO) and the Global Task Force on Cholera Control (GTFCC) – is one such concerted effort. This consortium, managed by and receiving technical guidance from the Agence de Médecine Préventive (AMP), is tasked with determining interventions and monitoring strategies for cholera elimination by 2030, generating additional momentum in the fight against cholera, particularly in Africa [2-4]. According to the WHO, more than 2.6 million cholera cases have been recorded in the last two decades, with over 60,000 deaths and a higher resurgence burden in Sub-Saharan Africa (SSA). The case fatality ratio (CFR) has persistently surpassed the recommended 1% by the WHO, averaging 2.2% annually and affecting an average of 23 different countries [5, 6].
Cholera is an acute diarrheal infection spread chiefly through contaminated water or food. Although mostly asymptomatic, severe cases present with dehydration, hypovolemic shock, and death in the absence of an immediate intervention [7]. Several risk factors contribute to disease transmission, including drinking contaminated water, ingesting infected food substances, poor environmental sanitation, and insufficient handwashing. Access to safe water, improved sanitation, hygiene promotion, timely and appropriate clinical case management, and the oral cholera vaccines encompass the prevention and control cascade [8]. The GTFCC targets a 90% reduction in cases and deaths by 2030, with continued efforts throughout Africa. Regional actions, such as establishing a WHO committee in 2018 and a ministerial meeting in 2023, demonstrate the continent’s commitment to increasing cholera prevention and response activities [5].
Regrettably, the year 2023 witnessed a threatening reemergence of cholera across the world, with alarming surges reported in at least 30 countries. The African region of the WHO recorded the highest number of resurgences with 17 countries reporting incidence in the year. This was closely followed by the Eastern Mediterranean Region, where 8 countries reported a resurgence. The American and South-East Asia Regions each reported a resurgence in two countries, while the Western Pacific Region had a country reporting an outbreak [9]. This recurrence raises public health concerns, given the strategic measures put in place by the GTFCC, such as constituting multisectoral cholera elimination plans [9]. The resurgence of cholera continues to have far-reaching adverse outcomes, impacting not just individual health but posing a significant strain on nations’ economies and existing fragile healthcare systems. By threatening the local economies of affected communities, it contributes to a cycle of poverty by instigating the diversion of developmental funds to manage outbreaks. In addition, the stigma attached to cholera-affected areas can discourage tourism and foreign investments, further impeding economic growth [10]. This perplexing trend and burden underscore the urgency and importance of delving into a comprehensive study on cholera in Africa, aiming to unravel the factors contributing to this resurgence and inform robust strategies for effective prevention and control to achieve the set target for 2030 [3]. Thus, this study aims to review the resurgence of cholera in Africa, by analyzing ongoing efforts, documenting progress made, identifying challenges faced and proposing evidence-based public health responses.
EPIDEMIOLOGY
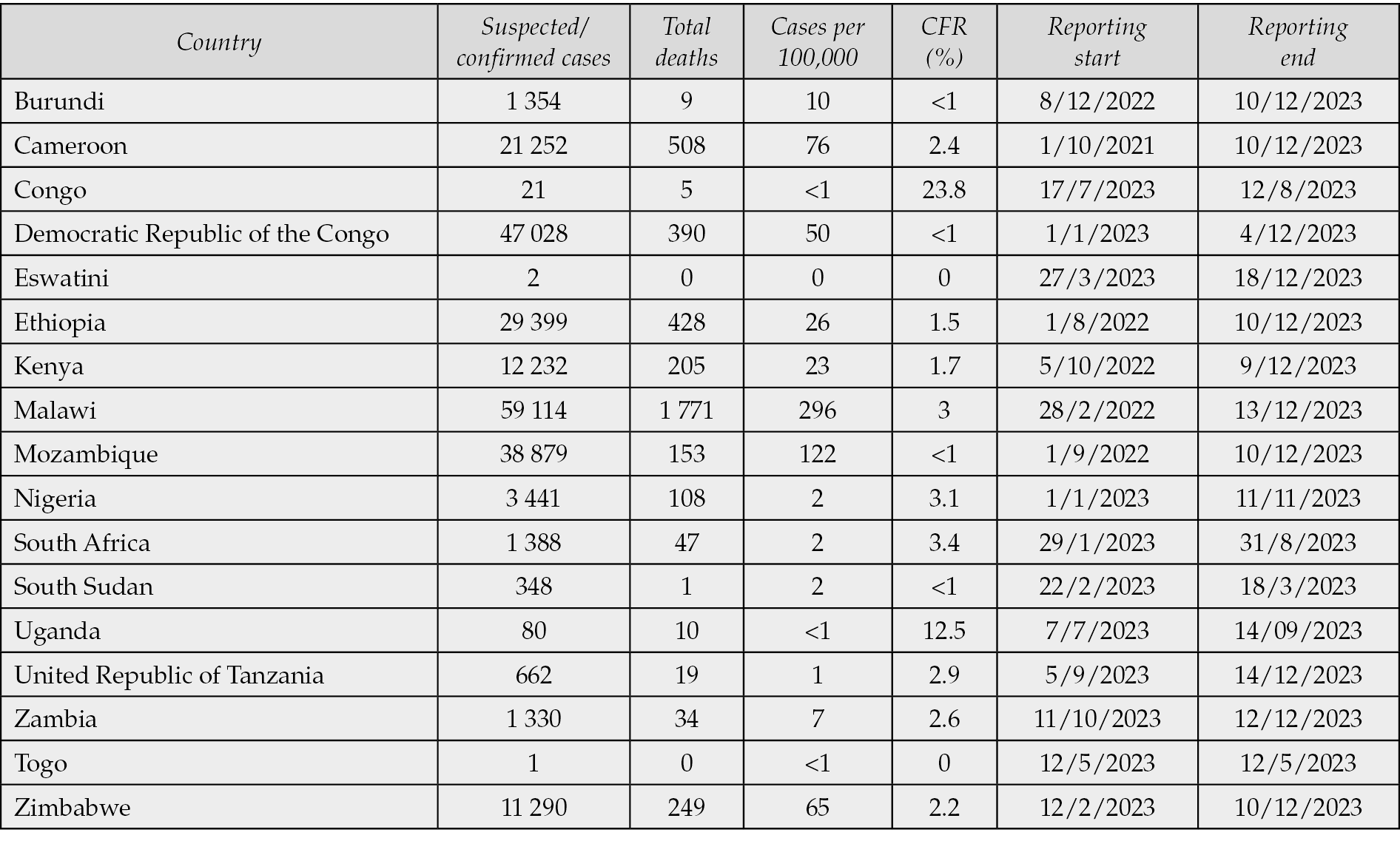
Between 2010 and 2019, sub-Saharan Africa accounted for 24% of the approximately 4.5 million cholera cases reported to the WHO [11]. For the period under review, epidemiological records documented 999 suspected cholera outbreaks, with over 480,000 probable patients spread across 744 separate sub-national regions in 25 African countries. From this pool, 128 sub-national areas reported confirmed cholera cases, while a little above 870 sub-national regions reported cholera-related deaths [11, 12]. In 2023, over 30 countries grappled with cholera resurgence – a double increment from those reported in 2022 and the first half of 2023. This heightened burden was also noted to cluster across Southeastern African states, particularly during the rainy season [13]. Preliminary data as of mid-December 2023 – for the period January to December 2023 – reported a staggering 667,000 cases and about 4,000 deaths across Malawi, Zimbabwe, the Democratic Republic of the Congo, Zambia, and Mozambique (Table 1) [14]. Malawi reported approximately 59,000 suspected/confirmed cases and above 1,700 deaths, which was the most in the region. Mozambique reported 38,879 cases and 153 deaths, while Zambia declared a new outbreak with 1,330 cases and 34 deaths. Zimbabwe recorded 11,290 cases and 249 deaths, and the Democratic Republic of the Congo reported 47,028 cases and 390 deaths. Ethiopia, grappling with heavy rainfall and displacement, reported 29,399 cases and 428 deaths, while Somalia documented 16,989 cases and 43 deaths. Sudan, amidst conflict, declared an outbreak with 6,739 cases and 200 deaths [14]. As of the 3rd week of 2024, six African nations – Burundi, Ethiopia, Kenya, the United Republic of Tanzania, Zambia, and Zimbabwe – had reported a total of 5,796 new cases of cholera with active transmission in 13 countries and no new case reported in Eswatini, the Democratic Republic of Congo (DRC), South Sudan, or Uganda. The WHO Regional Office for Africa (AFRO), as of January 21, 2024, had received reports of 17,614 cholera cases and 526 deaths, with a CFR of 3.0% [15].
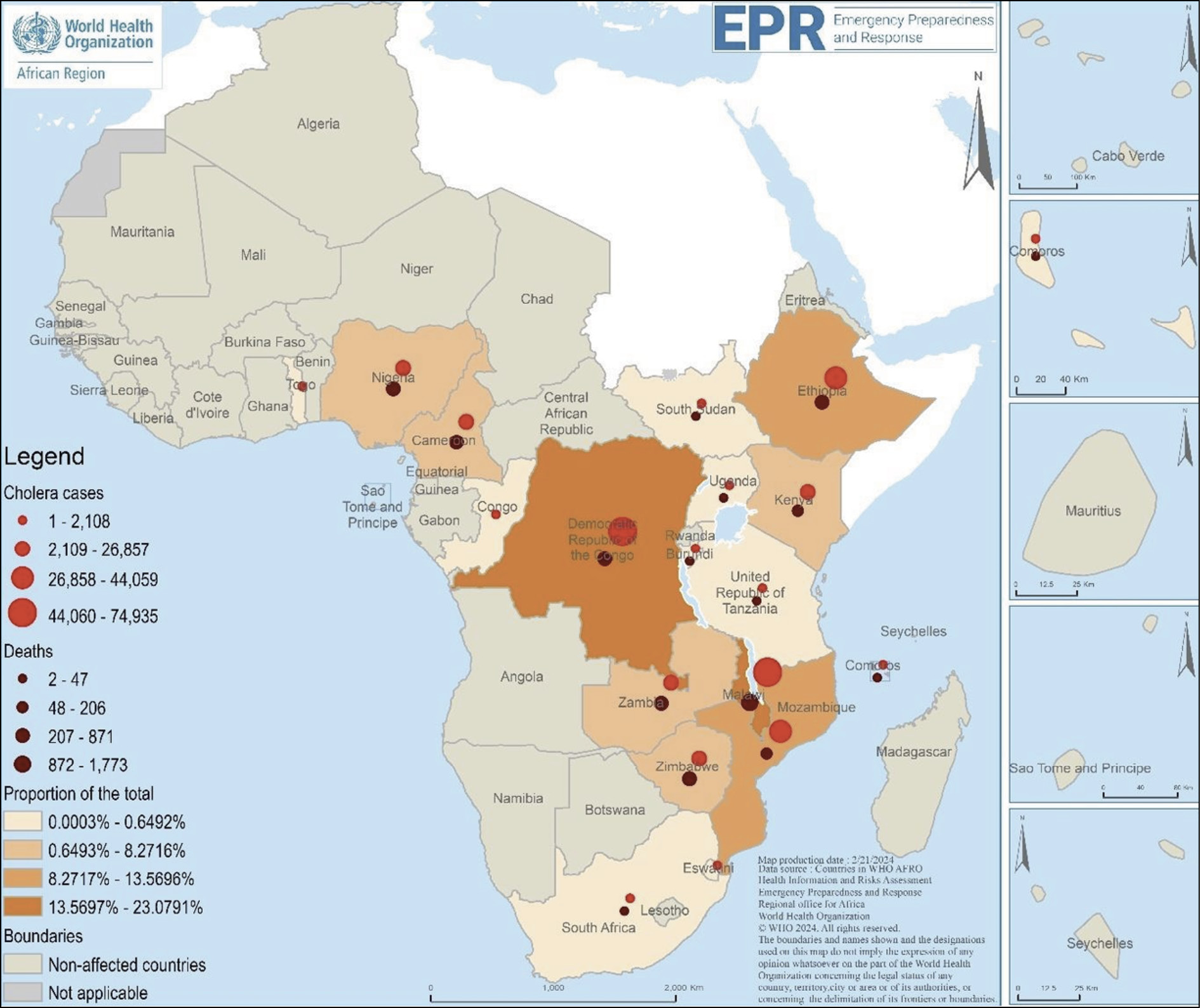
Figure 1 - Cholera cases and deaths in the WHO African Region between January 1, 2022 and February 18, 2024 [16]. Source: (WHO, 2024).
Table 1 - Outbreak of Cholera in Africa [14].
PROGRESS
The cholera eradication strategy in Africa consists of a comprehensive plan that includes awareness efforts and the reinforcement of water, sanitation, and hygiene (WASH) measures in affected communities [17]. Cholera treatment units have been built in all regions affected across the continent, equipped with the necessary supplies and diagnostic tools to enable timely management and prevention of possible deaths. The approach addresses water and sanitation issues through pot-to-pot chlorination, hygiene facility distribution, and the installation of prefabricated pit latrines and handwashing stations at treatment centers [18, 19]. The Ministry of Health (MOH) in Malawi and the United Nations International Children’s Emergency Fund (UNICEF) have collaboratively implemented community mobilization efforts, including sensitization campaigns, engagement of community leaders, and the construction of pit latrines [20]. In addition, they have expanded the surveillance system by deploying Health Surveillance Assistants and community volunteers to monitor, trace, discover, and report new cholera cases effectively. Community awareness campaigns are prevalent, with community leaders advocating health-seeking behaviors and enforcing local bylaws and action plans to combat the spread of cholera [21]. The inclusion and targeted deployment of oral cholera vaccines (OCVs) highlight landmark achievements in Africa’s cholera eradication efforts. Recognizing its efficacy in short-term prophylaxis, WHO advocates using the vaccine as an adjunct to existing water and sanitation programs [22, 23].
Currently, WHO has licensed and prequalified three OCVs, Dukoral, Shanchol, and Euvichol, in response to the cholera outbreak in Africa. Dukoral, which has been reported as the first prequalified OCV, comprises cholera toxin B-subunit (CTB) and inactivated whole cells of serogroup O1, with a sodium bicarbonate buffer to protect against gastric acid degradation [24]. In the 1980s, Swedish researchers enabled the transfer of strains and vaccine technology to Vietnam, leading to the development of a modified vaccine known as mORC-Vax. Although mORC-Vax could not be prequalified due to the Vietnamese NRA, the International Vaccine Institute (IVI) altered the formulation and moved the technique to India’s Shantha Biotechnics, Ltd., culminating in Shanchol’s prequalification in 2011 [25]. IVI also transferred the process to Eubiologics Co., Ltd. in South Korea, which prequalified Euvichol in 2015 after demonstrating safety and immunogenicity comparable to Shanchol in early-phase and non-inferiority trials [25, 26]. Traditional cholera vaccines used killed whole bacteria cells (WC). However, recent technological advances have allowed a combination of older technologies with newer ones, like recombinant technology, to create vaccines such as OraVacs. This enteric-coated capsule contains inactivated WC of Vibrio cholerae of specific biotypes and a recombinant cholera B subunit (rBS) [27]. OraVacs, like most other vaccines, is efficacious against cholera and traveler’s diarrhea and is delivered in three capsules on days 0, 7, and 28. Although clinical efficacy testing is still underway, safety and immunogenicity trials have shown effectiveness. OraVacs, now only available in the Philippines and China, shows promise for broader adoption [28]. This rBS-WC vaccine has been found to confer both herd immunity and direct effectiveness on susceptible residents in sub-Saharan Africa. Oral cholera vaccines have also been reported in Zanzibar to confer herd protection [29].
CHALLENGES IN CHOLERA PREVENTION AND CONTROL IN AFRICA
African countries continue to record worrisome cases of cholera, obscuring concerted efforts via immunization campaigns and other modalities. The present outbreak faces hurdles and is driven by a lack of safe WASH facilities, which has been compounded by a tropical storm that has damaged water sources and limited access to clean drinking water [21, 30]. Fluctuations in weather patterns, marked by heightened rainfall or prolonged droughts, significantly influence water sources and sanitation systems. The resulting shifts in climate conditions create an environment conducive for the proliferation and dissemination of cholera bacteria [31]. Furthermore, extreme weather events, variations in temperature and precipitation, and altered water patterns, exacerbated by increased flooding, contribute to the contamination of water sources, thereby facilitating the transmission of the disease [32, 33]. The lack of efficient human waste management is a critical problem for cholera eradication in Africa, with approximately 17% of the population engaging in open defecation and widespread use of inadequate shared bathroom facilities [21, 34]. Another key barrier is the presence of porous borders, which enables cross-migration and the importation of cholera cases, contributing to cross-border cholera epidemics in Sub-Saharan African countries [35]. Cross-border patient movements, inadequate risk assessment, and a lack of information exchange and coordination in conducting prevention initiatives between neighboring nations all compound cholera prevention and control challenges [36]. The ongoing cholera outbreak in Africa, and resultant deaths, underscore the deficit in the continent’s disease surveillance system. Delayed detection, reporting, and treatment of cholera cases in regions with high CFRs further support the reported weakened surveillance systems. The consequence is a continuous cross-territorial spread of the disease [21, 37].
Lack of awareness and education on proper sanitation practices contribute to the persistence of cholera. Communities limited understanding of how good hygiene and sanitation practices prevent cholera transmission can hinder preventive efforts. [23]. In remote and underserved areas, limited access to healthcare facilities and delayed medical intervention can result in higher mortality rates during outbreaks [38]. Cholera outbreaks strain already overburdened healthcare systems, exacerbated by the simultaneous occurrence of epidemics of other diseases such as dengue, measles, chikungunya, monkeypox (Mpox), and the present SARS CoV evolution [39]. The COVID-19 pandemic has further intensified the effect of the resurgence. Resource-strained healthcare systems and those yet to recover from the scourge of the pandemic still grapple with the provision of adequate sanitation and water treatment supplies across facilities, and densely populated areas. The ripple effect of healthcare workforce emigration post-pandemic across African countries has further intensified this burden. Furthermore, the focus on COVID-19 has diverted resources and attention away from other infectious diseases, leading to a decline in routine surveillance and early detection of cholera outbreaks. This delay has meted devastating consequences, even as cholera spreads rapidly in areas with inadequate hygiene infrastructure. Concerns about COVID-19 vaccines may extend to other immunization programs, potentially leading to lower vaccination rates for diseases such as measles or polio and increasing vulnerability within communities [40]. Multiple health crises pressure the overall capacity to respond to cholera, especially in nations with limited life resources. Insufficient medical facilities, shortages of medical personnel, and inadequate supplies further impede the ability to provide timely and effective care [34, 41]. Additional barriers include the emigration of both young and highly qualified physicians, disruptions in routine health services leading to the resurgence of the disease, difficulty accessing healthcare facilities, and assaults on healthcare providers, all of which impede outbreak response efforts [42-44]. Constant political instability, violence, insecurity, and significant migrations of people in the region put further strain on already inadequate social services, particularly in water and sanitation, increasing the risk of cholera outbreaks [45, 46].
Furthermore, the risk of transmission is raised in scenarios with large crowds, overcrowded environments, and restricted WASH programs, such as those seen among refugee and internally displaced persons (IDP) camps, as well as specific social activities during religious ceremonies [10, 47]. Many refugees and IDPs in the humanitarian-affected region live in congested camps with limited access to critical social services such as health, education, water, and sanitation. This disadvantaged population is prone to developing infectious illnesses such as cholera, as seen in ongoing conflict zones such as those in Sudan and Gaza [10, 48]. Noncompliance with the 2005 International Health Regulations (IHRs), particularly regarding cholera epidemic reporting in some countries – not declaring cholera outbreaks but reporting acute watery diarrhea (AWD) – violates the IHR’s intent. This denial results in the non-disclosure of test data and purposeful underreporting, which impedes effective efforts toward control and increases the frequency and severity of cholera epidemics [5, 49]. Another major impediment to cholera vaccination is the finnancial commitment required for large immunization programs targeting millions of people, as well as logistics challenges and issues surrounding cold chain management [50]. Achieving adequate vaccine coverage is difficult in environments with limited infrastructure, which is common in most sub-Saharan regions and worse during cholera outbreaks [51]. As previously highlighted by the WHO, technical difficulties have hampered the public health use of cholera vaccines, raising questions about their efficacy in the face of these obstacles [52].
RECOMMENDATION FOR PUBLIC HEALTH RESPONSE
To eliminate cholera in Africa by 2030, countries must actively adopt the WHO cholera roadmap. This comprehensive strategy, known as “Ending Cholera – A Global Roadmap to 2030”, is a collaborative effort among stakeholders, including cholera-affected countries, technical partners, and donors [2, 53]. The strategy aims to reduce cholera mortality by 90% and promote the elimination of disease transmission in as many countries as possible by 2030 [53]. This strategy focuses on three key areas: prompt detection and rapid response to outbreaks, a targeted multi-sectoral approach to cholera prevention, and an effective coordination mechanism for technical assistance, advocacy, resource mobilization, and partnerships at the local and global levels. Countries can make substantial progress in controlling and eventually eliminating cholera by improving community participation, boosting surveillance and laboratory capacities, implementing preventative measures in cholera hotspots, and developing a coordinated support network [54].
A multipronged approach is required to combat and eradicate cholera in Africa, including political commitment towards effective public health legislation against pro-cholera practices, water purification, hygiene standards, social mobilization, and oral cholera immunization [55, 56]. To avoid transmission of the disease, it is crucial to reduce contact with cholera patients, carry out proper disinfecting measures when in contact with a patient, hygienically handle sewage and fecal sludge, and promote good toilet habits [54]. To ensure sustained effectiveness and long-term control, it is imperative to establish a system for regular monitoring and inspection of sanitation facilities [57]. Public awareness initiatives, especially in endemic areas, are crucial. Campaigns should emphasize ongoing health promotions, focusing on decontaminating strategies through simple methods like boiling and chlorination, alongside promoting basic handwashing practices [58, 59]. Real-time surveillance, improved reporting, and prompt notification are critical in providing early alerts and enabling speedy response, particularly during seasonal outbreaks. Developing cutting-edge cholera intervention strategies, such as remote sensing technologies for satellite imagery and spatial clustering tools, and AI-powered data analysis tools incorporating machine learning algorithms, can be used to monitor environmental factors and predict higher-risk areas, while biosensors can improve diagnosis speed and accuracy, especially in the wake of technological advancements in epidemic response and control.
Furthermore, capacity building for primary and secondary health care providers (HCPs), especially on index case identification and high levels of suspicion, basic first aid responses such as rehydration plans and treatment protocols, and infection control strategies, is a condito sine qua non [33, 60]. Vaccination against cholera is highly recommended. Prequalified choices, including Dukoral, Sanchol, Euvichol, and the recombinant technology-based OraVacs, show efficacy and low side effects, making mass vaccination campaigns helpful in outbreak areas and hotspots [21, 54]. Travel medicine practitioners are vital in educating travelers about cholera risks, preventive measures such as vaccination and safe food and water practices. Additionally, they become invaluable at offering clinical and public health counsel with emergence of clinical symptoms. It is crucial to provide travelers with information on risk areas, preventive measures, and available preventive and curative healthcare resources. Considering cholera vaccination for travelers visiting high-risk areas in consultation with a healthcare professional is advisable. Prompt medical attention should be sought if symptoms consistent with cholera occur upon return. To prevent future epidemics, African governments must prioritize investments in WASH programs while actively promoting behavioral changes that improve sanitation practices [21, 49]. International organizations should help the African continent strengthen research and innovative interventions, emphasizing cholera epidemiology and developing evidence-based disease prevention and management policies [5, 21, 46].
CONCLUSIONS
In conclusion, eradicating the cholera outbreak in Africa requires a coordinated effort, backed by the GTFCC, to exchange technical experience and boost countries’ prevention and control capacities. Technical support for continuing epidemics, engagement with key partners, and leveraging resources for global surveillance are all critical. Surveillance should be improved by implementing rapid diagnostic tests and boosting laboratory capacities. Vaccination guidance, support for greater production, and identifying high-need areas are all emphasized. Case management has to be strengthened, and infection prevention and control activities should involve advocacy and resource mobilization. Risk communication and community participation strategies suited to local circumstances are essential, as are initiatives that enhance cleanliness and ensure the availability of water and sanitary facilities. These approaches are expedient to achieving the global 2030 elimination target in Africa.
Conflicts of interest
None.
Funding
No funding was received for this study.
Authors contributions
All authors contributed equally to the writing of this manuscript and I’ve read and approved the final draft.
REFERENCES
[1] Ajayi A, Smith SI. Recurrent cholera epidemics in Africa: which way forward? A literature review. Infection. 2019; 47(3): 341-349.
[2] GTFCC. ROADMAP TO 2030 A new global strategy to reduce cholera deaths and interrupt disease transmission. Available from: https://www.gtfcc.org/fr/a-propos-du-gtfcc/feuille-de-route-2030/. Accessed: December 15, 2023.
[3] Taty N, Bompangue D, Moore S, et al. Cholera resurgence potentially induced by the consequences of climate in the El Niño phenomenon: an urgent call for strengthened cholera elimination in Africa. Pan Afr Med. 2023; 46.
[4] Munier A, Njanpop-Lafourcade BM, Sauvageot D, et al. The African cholera surveillance network (Africhol) consortium meeting, 10-11 June 2015, Lomé, Togo. BMC Proc. 2017; 11 (Suppl. 1): 2. doi:10.1186/s12919-016-0068-z
[5] Olu OO, Usman A, Ameda IM, et al. The Chronic Cholera Situation in Africa: Why Are African Countries Unable to Tame the Well-Known Lion? Heal Serv Insights. 2023 Jan 14; 16.
[6] Uwishema O, Okereke M, Onyeaka H, et al. Threats and outbreaks of cholera in Africa amidst COVID-19 pandemic: a double burden on Africa’s health systems. Trop Med Health. 2021; 49(1): 93.
[7] Centers for Disease Control and Prevention (CDC). Cholera - Vibrio cholerae infection. Available from: https://www.cdc.gov/cholera/index.html. Accessed: December 16, 2023
[8] Qaserah AM, Al Amad MA, Al Serouri AA, Khader YS. Risk Factors of Cholera Transmission in Al Hudaydah, Yemen: Case-Control Study. JMIR Public Heal Surveill. 2021; 7(7): e27627.
[9] WHO. Weekly Bulletin on Outbreaks and other Emergencies: Week 40: 02 October - 08 October 2023 (Data as reported by: 17:00; 08 October 2023). Available from: https://reliefweb.int/report/ethiopia/weekly-bulletin-outbreaks-and-other-emergencies-week-40-02-october-08-october-2023-data-reported-1700-08-october-2023.
[10] Buliva E, Elnossery S, Okwarah P, Tayyab M, Brennan R, Abubakar A. Cholera prevention, control strategies, challenges and World Health Organization initiatives in the Eastern Mediterranean Region: A narrative review. Heliyon [Internet]. 2023; 9(5): e15598. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2405844023028050. Accessed: December 16, 2023.
[11] WHO Cholera 2022. Weekly epidemiological record 96 [Internet]. Available from: http://www.who.int/wer.
[12] Zheng Q, Luquero FJ, Ciglenecki I, et al. Cholera outbreaks in sub-Saharan Africa during 2010-2019: a descriptive analysis. Int J Infect Dis. 2022; 122: 215-221.
[13] WHO. Cholera in the WHO African Region: Weekly Regional Cholera Bulletin - 17 July 2023 [Internet]. 2023. Available from: https://www.afro.who.int/publications/cholera-who-african-region-weekly-regional-cholera-bulletin-29-march-2023-cloned. Accessed: December 16, 2023.
[14] World Health Organisation. Multi-country outbreak of cholera, External situation report #10 - 11. 2024 Jan 11[cited 2024 February 6]; Available from: https://www.who.int/publications/m/item/multi-country-outbreak-of-cholera--external-situation-report--10---11-january-2024. Accessed: February 6, 2024.
[15] WHO. Weekly Regional Cholera Bulletin: 22 January 2024 [Internet]. Available from: https://www.afro.who.int/health-topics/disease-outbreaks/cholera-who-african-region#:~:text=In 2024%2C the number of case fatality ratio of 3.0%25. Accessed February7, 2024.
[16] WHO. Weekly Regional Cholera Bulletin: 19 February 2024 [Internet]. Available from: https://iris.who.int/bitstream/handle/10665/376113/AFRO%20Cholera%20Bulletin.52.pdf Accessed March 7, 2024.
[17] Bagcchi S. Malawi takes on cholera outbreak amid cyclone devastation. The Lancet Microbe. 2022; 3(7): e480.
[18] D’Mello-Guyett L, Gallandat K, Van den Bergh R, et al. Prevention and control of cholera with household and community water, sanitation and hygiene (WASH) interventions: A scoping review of current international guidelines. Azman AS, editor. PLoS One. 2020; 15(1): e0226549.
[19] Lantagne D, Yates T. Household Water Treatment and Cholera Control. J Infect Dis. 2018; 218 (Suppl. 3): S147-153.
[20] Unicef Malawi. UNICEF and WHO step up efforts to contain Cholera in Malawi and call for additional funds and support, 2022 [Internet]. Available from: https://www.unicef.org/malawi/press-releases/unicef-and-who-step-efforts-contain-cholera-malawi-and-call-additional-funds-and Accessed December 17, 2023
[21] Miggo M, Harawa G, Kangwerema A, et al. Fight against cholera outbreak, efforts and challenges in Malawi. Heal Sci Reports. 2023; 6(10).
[22] M’bangombe M, Pezzoli L, Reeder B, et al. Oral cholera vaccine in cholera prevention and control, Malawi. Bull World Health Organ. 2018; 96(6): 428-435.
[23] Trolle H, Forsberg B, King C, et al. A scoping review of facilitators and barriers influencing the implementation of surveillance and oral cholera vaccine interventions for cholera control in lower- and middle-income countries. BMC Public Health. 2023; 23(1): 455.
[24] Baik YO, Choi SK, Olveda RM, et al. A randomized, non-inferiority trial comparing two bivalent killed, whole cell, oral cholera vaccines (Euvichol vs Shanchol) in the Philippines. Vaccine. 2015; 33(46): 6360-6365.
[25] Wierzba TF. Oral cholera vaccines and their impact on the global burden of disease. Hum Vaccin Immunother. 2019; 15(6): 1294-1301.
[26] Baik YO, Choi SK, Kim JW, et al. Safety and Immunogenicity Assessment of an Oral Cholera Vaccine through Phase I Clinical Trial in Korea. J Korean Med Sci. 2014; 29(4): 494.
[27] Lopez AL, Gonzales MLA, Aldaba JG, Nair GB. Killed oral cholera vaccines: history, development and implementation challenges. Ther Adv Vaccines. 2014; 2(5): 123-136.
[28] Shaikh H, Lynch J, Kim J, Excler JL. Current and future cholera vaccines. Vaccine. 2020; 38: A118-126.
[29] Khatib AM, Ali M, von Seidlein L, et al. Effectiveness of an oral cholera vaccine in Zanzibar: findings from a mass vaccination campaign and observational cohort study. Lancet Infect Dis. 2012; 12(11): 837-844.
[30] Sow AU, Haruna UA, Amos OA, et al. Tackling Cholera Outbreak Amidst COVID-19 Pandemic in Nigeria: challenges and recommendations. Public Health Rev. 2022; 43.
[31] Duchenne-Moutien RA, Neetoo H. Climate Change and Emerging Food Safety Issues: A Review. J Food Prot. 2021; 84(11): 1884-1897.
[32] Christaki E, Dimitriou P, Pantavou K, Nikolopoulos GK. The Impact of Climate Change on Cholera: A Review on the Global Status and Future Challenges. Atmosphere (Basel). 2020; 11(5): 449.
[33] Davis W, Narra R, Mintz ED. Cholera. Curr Epidemiol Reports. 2018; 5(3): 303-315.
[34] Somboonwit C, Menezes LJ, Holt DA, Sinnott JT, Shapshak P. Current views and challenges on clinical cholera. Bioinformation. 2017; 13(12): 405-409.
[35] Challa JM, Getachew T, Debella A, et al. Inadequate hand washing, lack of clean drinking water and latrines as major determinants of cholera outbreak in Somali Region, Ethiopia in 2019. Front Public Heal. 2022; 10. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.845057/full
[36] Bwire G, Mwesawina M, Baluku Y, Kanyanda SSE, Orach CG. Cross-border cholera outbreaks in Sub-Saharan Africa, the mystery behind the silent illness: what needs to be done? Carpenter DO, editor. PLoS One. 2016; 11(6): e0156674.
[37] Fagbamila IO, Abdulkarim MA, Aworh MK, et al. Cholera outbreak in some communities in North-East Nigeria, 2019: an unmatched case-control study. BMC Public Health 2023; 23(1): 446.
[38] Azevedo MJ. The State of Health System(s) in Africa: Challenges and Opportunities. In 2017. p. 1-73. Available from: https://link.springer.com/10.1007/978-3-319-32564-4_1
[39] Mohapatra RK, Kutikuppala LVS, Kandi V, Mishra S, Tuglo LS, Dhama K. Recent surge in cholera outbreaks globally during the COVID-19 pandemic era: a potential threat to the African continent and salient counteracting strategies. Int J Surg. 2023; 109(3): 631-633.
[40] Ali I. Impact of COVID-19 on vaccination programs: adverse or positive? Hum Vaccines Immunother. 2020 Nov 1 [cited 2024 Mar 9]; 16(11): 2594-2600. Available from: https://doi.org/10.1080/21645515.2020.1787065
[41] Omosigho PO, Okesanya OJ, Olaleke NO, Eshun G, Lucero-Prisno DE. Multiple burden of infectious disease outbreaks: Implications for Africa healthcare system. J Taibah Univ Med Sci. 2023; 18(6): 1446-1448.
[42] Arage MW, Kumsa H, Asfaw MS, et al. Exploring the health consequences of armed conflict: the perspective of Northeast Ethiopia, 2022: a qualitative study. BMC Public Health. 2023; 23(1): 2078.
[43] Eltvedt AK, Poulsen A, Winther TN, Von Linstow ML. Barriers for vaccination of healthcare workers. Hum Vaccin Immunother. 2021; 17(9): 3073-3076.
[44] Daniel FM, Essien EA, Gbuchie MA, Ukoaka BM, Emeruwa VE. Mitigating physician emigration in Nigeria by improving the internship experience. IJMS. 2023; 11(4): 343-346.
[45] Clemens JD, Nair GB, Ahmed T, Qadri F, Holmgren J. Cholera. Lancet. 2017; 390(10101): 1539-1549.
[46] Deen J, Mengel MA, Clemens JD. Epidemiology of cholera. Vaccine. 2020; 38: A31-40.
[47] Camacho A, Bouhenia M, Alyusfi R, et al. Cholera epidemic in Yemen, 2016-18: an analysis of surveillance data. Lancet Glob Heal. 2018; 6(6): e680-90.
[48] Sparrow A, Almilaji K, Tajaldin B, Teodoro N, Langton P. Cholera in the time of war: implications of weak surveillance in Syria for the WHO’s preparedness - a comparison of two monitoring systems. BMJ Glob Heal. 2016; 1(3): e000029.
[49] Musa SS, Ezie KN, Scott GY, et al. The challenges of addressing the cholera outbreak in Cameroon. Public Heal Pract. 2022: 100295.
[50] Date K, Vicari A, Hyde T, Mintz E, et al. Considerations for oral cholera vaccine use during outbreak after earthquake in Haiti, 2010-2011. Emerg Infect Dis]. 2011; 17(11).
[51] Chaignat CL, Monti V. Use of oral cholera vaccine in complex emergencies: what next? Summary report of an expert meeting and recommendations of WHO. J Health Popul Nutr. 2007; 25(2): 244-261.
[52] von Seidlein L, Jiddawi M, Grais RF, Luquero F, Lucas M, Deen J. The value of and challenges for cholera vaccines in Africa. J Infect Dis. 2013; 208 (Suppl. 1): S8-14.
[53] Global Task Force on Cholera Control. Ending cholera. A Global Roadmap to 2030. World Health Organization; 2017 [Internet]. Available from: https://www.who.int/cholera/publications/global-roadmap/en/ Accessed: January 13, 2024.
[54] Ayenigbara IO, Ayenigbara GO, Adeleke RO. Contemporary Nigerian public health problem: prevention and surveillance are key to combating cholera. GMS Hyg Infect Control. 2019; 1 4: Doc 16.
[55] Control. WHOE and other CDS and. WHO guidance on formulation of national policy on the control of cholera. WHO/CDD/SER/92.16 REV.1. 1992. Available from: https://www.who.int/topics/cholera/publications/WHO_CDD_SER_92_16/en/ Accessed January 12, 2023.
[56] Purdy AE. Fly Models of Vibrio cholerae Infection and Colonization. In 2018. p. 77–96. Available from: http://link.springer.com/10.1007/978-1-4939-8685-9_8 Accessed January, 12, 2023
[57] Ebi KL, Hess JJ, Watkiss P. Health Risks and Costs of Climate Variability and Change. Dis Control Priorities, Third Ed (Volume 7) Inj Prev Environ Heal. 2017; 153-169.
[58] Zhang Y, Sivakumar M, Yang S, Enever K, Ramezanianpour M. Application of solar energy in water treatment processes: A review. Desalination. 2018; 428: 116-145.
[59] Gidado S, Awosanya E, Haladu S, et al. Cholera outbreak in a naïve rural community in Northern Nigeria: the importance of hand washing with soap, September 2010. Pan Afr Med J. 2018; 30.
[60] Spiegel P, Ratnayake R, Hellman N, et al. Responding to epidem ics in large-scale humanitarian crises: a case study of the cholera response in Yemen, 2016-2018. BMJ Glob Heal. 2019; 4(4): e001709.