Le Infezioni in Medicina, n. 2, 131-137, 2024
doi: 10.53854/liim-3202-2
REVIEWS
Meta-meta-analysis of the mortality risk associated with MRSA compared to MSSA bacteraemia
Shuaibu Suleiman Adeiza1,2, Islam Aminul3,4
1Dept of Pharmaceutical Microbiology & Biotechnology, Faculty of Pharmaceutical Sciences, Ahmadu Bello University, Zaria, Nigeria;
2Dept of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmaceutical Sciences, Usmanu Dafodiyo University Sokoto, Nigeria;
3Advanced Molecular Laboratory, Department of Microbiology, President Abdul Hamid Medical College, Karimganj, Kishoreganj-2310, Bangladesh;
4COVID-19 Diagnostic Laboratory, Department of Microbiology, Noakhali Science and Technology University, Noakhali, Bangladesh
Article received 25 January 2024, accepted 8 April 2024
Corresponding author
Suleiman Adeiza Shuaibu
E-mail: Suleykestler2@gmail.com
SummaRY
Staphylococcus aureus bacteraemia (SAB) is a bloodstream infection that carries a high risk of exacerbating a diseased state and may result in an increased death rate. The aim of this study was to assess mortality risk in Methicillin Resistant Staphylococcus aureus (MRSA) bacteraemia compared to Methicillin Susceptible Staphylococcus aureus (MSSA) bacteraemia through meta-meta-analyses. The study followed PRISMA guidelines, conducting a comprehensive search in Scopus, PubMed, and Google Scholar. It included full-text systematic reviews and meta-analyses comparing MRSA vs. MSSA bacteraemia, excluding reviews without data pooling and unclear selection criteria. Validity was assessed using QUOROM and AMSTAR. Edwards’ Venn diagrams were used to visualized overlaps between primary studies. Aggregated odds ratio (OR) and risk ratios with 95% confidence intervals were calculated using the random-effect model. Heterogeneity was evaluated using the Higgins I2 statistic. The study included 3 meta-analysis studies, a total of 38,159 patients, with 9,056 having MRSA bacteraemia and 29,103 having MSSA bacteraemia. Data were collected from 46 different outcome studies published between 2001 and 2022. The meta-analyses used 7 to 33 primary studies from 1990 to 2020, with no overlap. Odds ratios (ORs) ranged from 1.78 to 2.92, while relative risks (RR) ranged from 1.57 to 2.37 for the included meta-anlysis. The pooled analysis confirmed a higher risk of mortality in patients with MRSA bacteraemia (OR: 2.35, RR: 2.01, HR: 1.61) compared to MSSA bacteraemia. Heterogeneity among the studies was considerable (I2: 90-91%).
The study strongly supports that most patient deaths from SAB are linked to MRSA rather than MSSA. This highlights the significant public health problem posed by SAB, with difficult and often unsuccessful treatment leading to increased mortality and high healthcare costs.
Keywords: Evidence synthesis, meta-analyses,MRSA, MSSA, Staphylococcus aureus bacteraemia.
INTRODUCTION
Staphylococcus aureus bacteraemia (SAB) is a bloodstream infection that carries a high risk of exacerbating a diseased state and may result in an increased death rate [1]. MRSA-related deaths result from acute complications like septic shock, coagulation issues, or lung injury, as well as complications of endocarditis or underlying disease [2]. Treatment of Methicillin-Resistant Staphylococcus aureus (S. aureus) or MRSA infections can be challenging due to limited antibiotic options, and in some cases, the infection may not respond well to available treatments [3]. This resistance to common antibiotics can lead to longer hospital stays, increased healthcare costs, and a higher risk of complications and death [4]. It’s important to note that both MRSA and Methicillin-Susceptible S. aureus (MSSA) bacteraemia are serious conditions that require immediate medical attention [4]. Prompt diagnosis and appropriate treatment, including the use of effective antibiotics, are essential for improving outcomes and reducing the risk of severe complications or death [5]. The risk of death from MRSA bacteraemia is generally higher compared to MSSA bacteraemia [6]. MRSA strains are resistant to methicillin and related drugs, which makes them more difficult to treat, leading to increased mortality rates [6]. Several studies have shown that patients with MRSA bacteraemia have higher mortality rates compared to those with MSSA bacteraemia [7]. The exact difference in mortality rates can vary depending on factors such as the patient population, the severity of illness, and the presence of underlying health conditions [7].
The aim of this study was to assess the mortality risk in MRSA bacteraemia compared to MSSA bacteraemia through meta-meta-analyses with the goal of improving evidence-based decision-making regarding the associated mortality risk.
METHODS
Criteria for inclusion and exclusion, along with the parsing of data
The study followed the PRISMA guidelines in conducting a literature review. A comprehensive search in three databases were carried out: Scopus, PubMed, and Google Scholar [13]. The search terms were; ((“risk”[MeSH Terms] OR “risk”[All Fields]) AND “odds”[All Fields] AND (“death”[MeSH Terms] OR “death”[All Fields] OR “deaths”[All Fields]) AND (“mortality”[MeSH Terms] OR “mortality”[All Fields] OR “mortalities”[All Fields] OR “mortality”[MeSH Subheading]) AND (“methicillin resistant staphylococcus aureus”[MeSH Terms] OR (“methicillin resistant”[All Fields] AND “staphylococcus”[All Fields] AND “aureus”[All Fields]) OR “methicillin resistant staphylococcus aureus”[All Fields] OR “mrsa”[All Fields]) AND “MSSA”[All Fields] AND (“bacteraemia”[All Fields] OR “bacteremia”[MeSH Terms] OR “bacteremia”[All Fields] OR “bacteraemias”[All Fields] OR “bacteremias”[All Fields])) AND (clinical trial[Filter] OR meta-analysis[Filter] OR randomized controlled trial[Filter] OR review[Filter] OR systematic review[Filter]).
This review focused on systematic reviews and meta-analyses that compared MRSA and MSSA bacteraemia using pooled data. Two authors (SA and AI) conducted a thorough assessment of potential studies, identifying relevant titles and abstracts with no disagreements between them. The review had no limitations based on the setting type or year of publication. The review included only full-text systematic reviews and meta-analyses of randomized controlled trials (RCT) that provided pooled data on MRSA vs MSSA bacteraemia. Excluded studies were reviews without data pooling, specified search algorithms, and clear selection criteria for included studies. The study protocol is registered with the open science framework (osf.io/dw8xm).
Data extracted from the included meta-analyses covered the study name, publication year, dichotomous number of events in each group, effect size data (Risk Ratio or Odds Ratio), number of databases searched, and review year range [8]. The validity and robustness of the included meta-analyses were assessed using the Quality of Reporting of Meta-analyses (QUOROM) checklist and Assessment of Multiple Systematic Reviews (AMSTAR) [9].
To visualize overlaps between primary studies, Edwards’ Venn diagrams were employed with the intervene shiny package in R studio (Version II). The aggregated odds ratio (OR) and risk ratios, along with their corresponding 95% confidence intervals (CI), were calculated using the random-effect model of DerSimonian and Laird, utilizing the ‘metafor’ package and Comprehensive meta-analysis software (version 3.0). Heterogeneity was assessed using the Higgins I2 statistic, with values below 25% indicating low heterogeneity and values above 75% indicating high heterogeneity [10].
Table 1 - Characteristics of included meta-analysis.
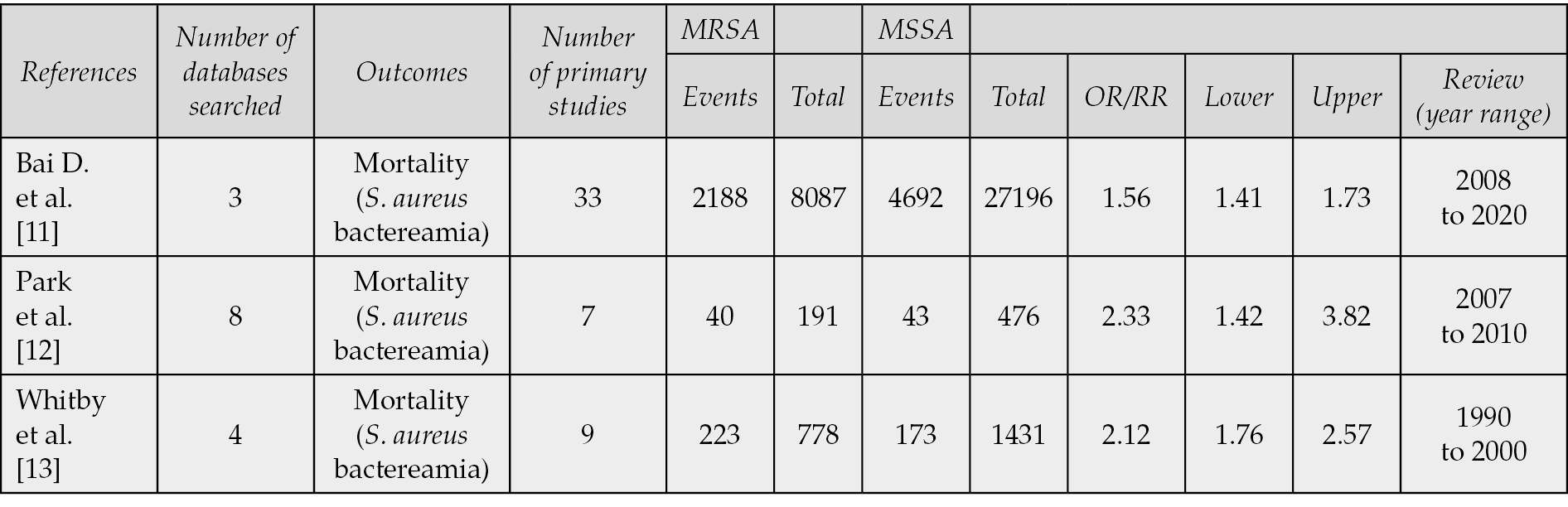
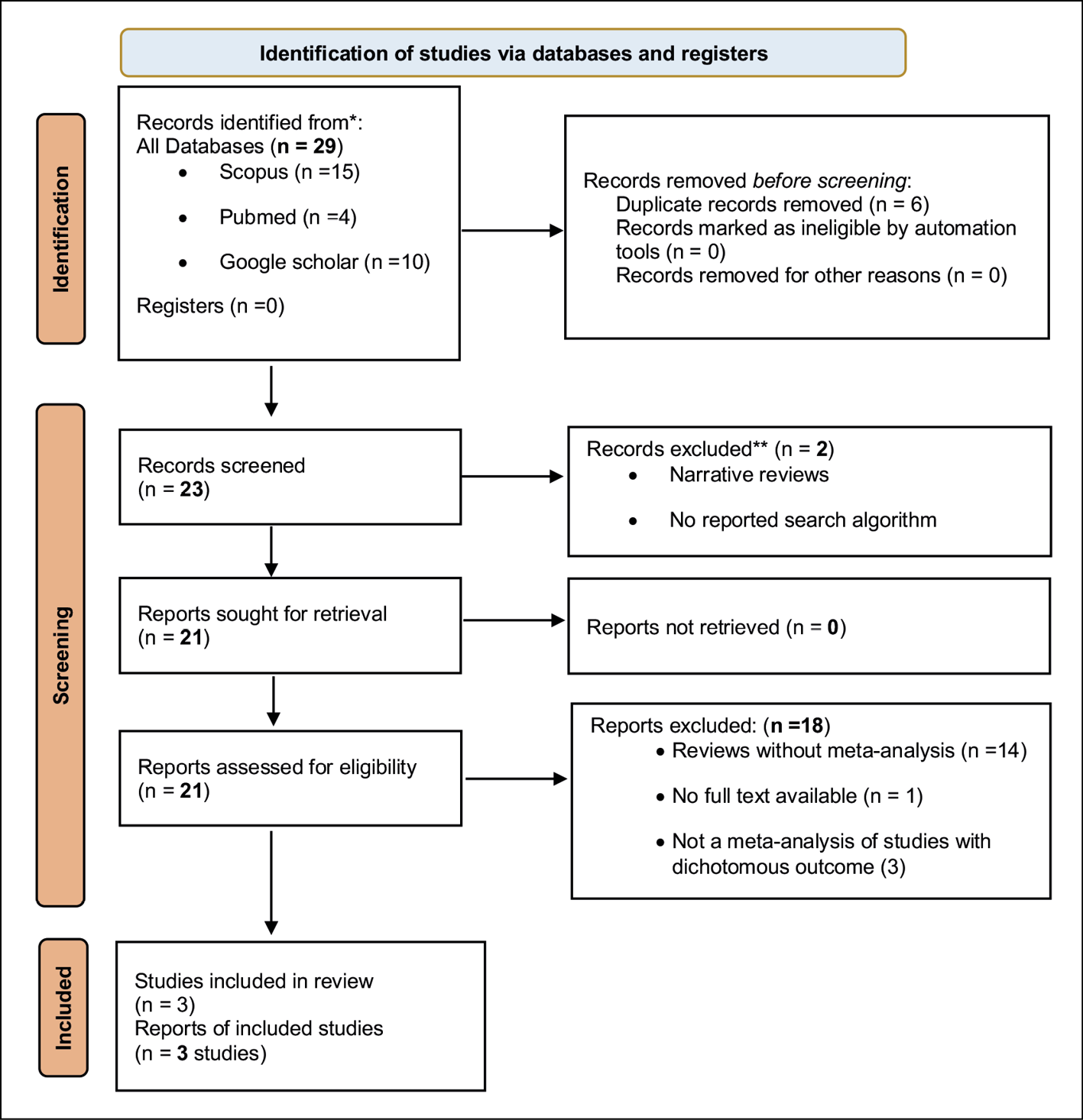
Figure 1 - PRISMA flow diagram of article Selection for inclusion.
RESULTS
Three meta-analysis were included in this study comprising a total of 38,159 patients [11-13]. These patients were divided into two groups: 9,056 patients with MRSA bacteraemia and 29,103 with MSSA bacteraemia. The data were collected from 46 different dichotomous outcome studies published between 2001 and 2022. The primary studies included in these meta-analyses were spanned from 1990 to 2020, with each meta-analysis comprising seven to thirty-three primary studies. There was no overlap in the primary studies used across the included meta-analyses.
The odds ratios (ORs) in the meta-analyses ranged mostly from 1.78 (95% CI, 1.68-1.89) to 2.92 (95% CI, 2.34-3.65), while the calculated relative risks (RR) ranged from 1.57 (95% CI, 1.50-1.64) to 2.37 (95% CI, 1.98-2.38). The AMSTAR score ranged from 14 to 15, and the QUOROM score ranged from 9-10.
The combined odds ratio (OR) from the pooled analysis was 2.35 (95% CI, 1.58-3.49, p=0.00), indicating a significantly higher odds of mortality in patients with MRSA bacteraemia compared to MSSA bacteraemia. Similarly, the pooled relative risk (RR) was 2.01 (95% CI, 1.43-2.81, p=0.00), suggesting a significantly higher risk of mortality in patients with MRSA bacteraemia compared to MSSA bacteraemia. Further, a pooled hazard ratio (HR) of 1.61 (95% CI, 1.53-1.70, p=0.00) was calculated.
The pooled analysis revealed considerable heterogeneity between the studies, with a χ2 value of 22.69 (p=0.00) and an I2 value of 91% for RR, and a χ2 value of 20.31 (p=0.00) and an I2 value of 90% for OR.
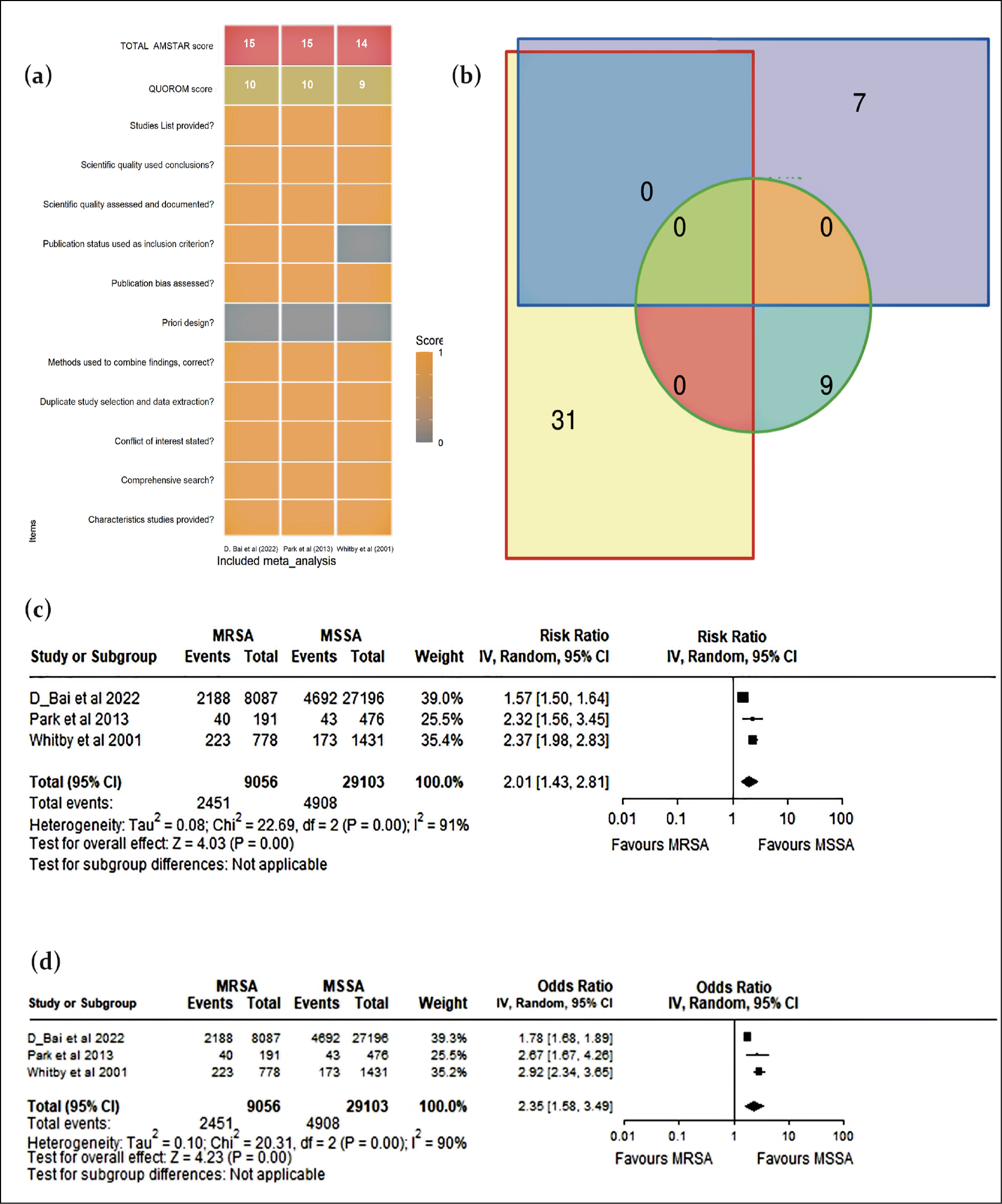
Figure 2 - (a) QUOROM and AMSTAR scores for the meta-analyses that were included in the study. (b) Edwards’ Venn diagrams, which illustrate the overlap of studies in the analysis. (c) A forest plot of the Risk Ratio (RR) of MRSA (Methicillin-resistant Staphylococcus aureus) versus MSSA (Methicillin-sensitive Staphylococcus aureus) bacteremia.(d) Another forest plot presenting the Odds Ratio (OR) of MRSA versus MSSA bacteremia.
DISCUSSION
The aim of this study was to systematically compile the evidence from multiple meta-analyses regarding mortality risk associated with MRSA compared to MSSA bacteraemia into an accessible up-to-date source. Three meta-analyses were identified and included in the review, [11-13]. The consistent finding across all three meta-analyses was a significantly higher mortality risk in MRSA bacteraemia compared to MSSA bacteraemia. The primary variation among the meta-analyses was in the magnitude of risk and odds. Combining the results of these meta-analyses yielded an overall substantial relative risk (RR) of 2.01 and an odds ratio (OR) of 2.35. These results demonstrate the consistency of conclusions across each individual meta-analysis.
Furthermore, two studies have reported RRs and ORs that align with our findings or fall within the range of the 95% confidence interval reported here [14, 15]. The increased mortality risk associated with MRSA bacteraemia is attributed to several factors, including limited treatment options: MRSA’s resistance to multiple antibiotics makes it more difficult to treat effectively [16]. The standard first-line antibiotics used to treat MSSA infections, such as methicillin and penicillin, are ineffective against MRSA. As a result, clinicians must rely on alternative, often more toxic or less effective antibiotics, which may not completely eradicate the infection [17]. Identifying MRSA requires specific laboratory testing, and the results may not be available for a few days especially in low income countries. Patients may receive broad-spectrum antibiotics that do not target MRSA effectively [18]. Delayed administration of appropriate antibiotics can lead to worsened outcomes. Some studies suggest that certain MRSA strains might have increased virulence compared to MSSA strains [16]. These strains can cause more severe infections, leading to a higher risk of complications and mortality [16]. MRSA is often associated with healthcare settings, such as hospitals and long-term care facilities [19]. Patients in these settings may already have weakened immune systems or other underlying health issues, making them more susceptible to severe infections [20]. MRSA strains have also emerged in community settings, affecting otherwise healthy individuals [21]. Community-acquired MRSA can cause severe infections, such as skin and soft tissue infections, which can lead to bacteraemia and, in some cases, mortality [22]. Patients who acquire MRSA bacteraemia often have other underlying health conditions that can complicate treatment and increase the risk of mortality [23]. It’s essential to recognize that while MRSA bacteraemia carries a higher risk of mortality compared to MSSA, the actual outcome can vary significantly depending on the patient’s overall health, the virulence of the infecting strain, and timely and appropriate medical intervention [24]. Early detection, appropriate antimicrobial therapy, and supportive care play crucial roles in improving the prognosis for patients with MRSA bacteraemia [23].
This analysis has limitations that should be acknowledged. Being a meta-analysis based on previously published articles and observational data, it limits the transparency and reproducibility of the study. Relying on existing literature also restricts individual patient data analysis and may lead to variations and potential biases. The diverse healthcare settings of the selected studies result in heterogeneous patient care. Caution is necessary when interpreting the results. To improve reliability and strengthen the evidence, further research using well-planned randomized controlled trials, including studies from the previous meta-analysis and other published works not previously considered, is needed.
CONCLUSIONS
The combined findings from comparing mortality rates provide strong evidence (based on Risk, odds, and Hazard Ratio) that the majority of patient deaths related to SAB were associated with MRSA rather than MSSA. This study’s evidence reinforces the notion that SAB poses a significant public health issue due to the challenging and often unsuccessful treatment, leading to increased mortality and imposing excessive costs on healthcare services.
Funding
None received.
Conflict of interest
The authors declared that they have no conflict of interest.
Authors contribution
S.A.S. played a key role in conceptualization, data curation, formal analysis, investigation, methodology and the original draft and subsequent revisions of the manuscript. A.I. contributed significantly to methodology development, resource allocation, software implementation, supervision, validation, and the critical review and editing of the manuscript.
Data availability
The data supporting the results of this study are openly accessible in the Open Science Framework (OSF) registries (osf.io/v7uz2), Supplementary documents, and available from the corresponding author upon request.
REFERENCES
[1] Parsons JB, Westgeest AC, Conlon BP, et al. Persistent Methicillin-Resistant Staphylococcus aureus bacteremia: host, pathogen, and treatment. Antibiotics 2023; 12: 455.
[2] Rodriguez-Quick VA, Llop A, Dimas K, et al. MRSA in the bursa: an unusual complication of MRSA bacteremia causing bilateral acromioclavicular septic arthritis. Access Microbiol. 2022; 4: acmi000438.
[3] Gao Y, Chen Y, Cao Y, et al. Potentials of nanotechnology in treatment of methicillin-resistant Staphylococcus aureus. Europ J Med Chem. 2021; 213: 113056.
[4] Davis JS, Petersiel N, Tong SYC. How I manage a patient with MRSA bacteraemia. Clin Microbiol Infect. 2022; 28: 190-194.
[5] Schwalb A, Cachay R, de la Flor A, et al. Adherence to standards of care and mortality in the management of Staphylococcus aureus bacteraemia in Peru: A prospective cohort study. Int J Infect Dis. 2020; 96: 601-606.
[6] Selvey LA, Whitby M, Johnson B. Nosocomial methicillin-resistant Staphylococcus aureus bacteremia: is it any worse than nosocomial methicillin-sensitive Staphylococcus aureus bacteremia? Infect Contr Hosp Epidemiol. 2000; 21: 645-648.
[7] Kim S-H, Jeon M, Jang S, et al. Factors for mortality in patients with persistent Staphylococcus aureus bacteremia: The importance of treatment response rather than bacteremia duration. J Microbiol Immunol Infect. 2023; 56(5): 1007-1015. doi: 10.1016/j.jmii.2023.07.010. Epub 2023 Jul 31.
[8] Suleiman AS, Islam MdA, Akter MS, et al. A meta-meta-analysis of co-infection, secondary infections, and antimicrobial resistance in COVID-19 patients. J Infect Public Health. Epub ahead of print 17 July 2023. doi: 10.1016/j.jiph.2023.07.005.
[9] Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009; 62: 1013-1020.
[10] Adeiza SS, Shuaibu Bello A, Shuaibu MG. Random effects meta-analysis of COVID-19/S. aureus partnership in co-infection. SSRN Journal. Epub ahead of print 2020. doi: 10.2139/ssrn.3724705.
[11] Bai AD, Lo CKL, Komorowski AS, et al. Staphylococcus aureus bacteraemia mortality: a systematic review and meta-analysis. Clin Microbiol Infect. 2022; 28: 1076-1084.
[12] Park DA, Lee SM, Peck KR, et al. Impact of Methicillin-Resistance on mortality in children and neonates with Staphylococcus aureus bacteremia: A meta-analysis. Infect Chemother 2013; 45: 202-210.
[13] Whitby M, McLaws M, Berry G. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: a meta-analysis. Med J Australia. 2001; 175: 264-267.
[14] Wang F-D, Chen Y-Y, Chen T-L, et al. Risk factors and mortality in patients with nosocomial Staphylococcus aureus bacteremia. Am J Infect Contr. 2008; 36: 118-122.
[15] Sinclair MR, Souli M, Ruffin F, et al. Staphylococcus aureus bacteremia among patients receiving maintenance hemodialysis: trends in clinical characteristics and outcomes. Am J Kidney Dis. 2022; 79: 393-403.
[16] Hsieh RC, Liu R, Burgin DJ, et al. Understanding mechanisms of virulence in MRSA: implications for antivirulence treatment strategies. Expert Rev Anti-infective Ther. 2023; 0: 1-18.
[17] Cinquegrani M, Cei F, Pistoia M, et al. MRSA bacteremia and new-onset aortic and mitral regurgitation: a pernicious and tricky association. Ital J Med. 17. Epub ahead of print 19 July 2023. doi: 10.4081/itjm.2023.1618.
[18] Xia J, Xin L, Li J, et al. Discovery of Quaternized Pyridine-Thiazole-Pleuromutilin derivatives with broad-spectrum antibacterial and potent Anti-MRSA activity. J Med Chem. 2023; 66: 5061-5078.
[19] Suleiman AS, Abbass M, Hossain M, Choudhary P, Bhattacharya P, Islam MA. Impact of antibiotic-coated sutures on surgical site infections: a second-order meta-analysis. Int J Surg. 2024; 110(1): 507-519.
[20] Shuaibu AS, Ibrahim YKE, Olayinka BO, et al. Aerobic bacteria from surgical wound infections in obstetrics and gynecology ward in specialist hospital Sokoto-North West Nigeria. Asian J Med Heal 2017; 3: 1-6.
[21] Amdan NN, Zamri HF, Ali MM, et al. Predominance of SCCmec type IV in community-acquired meticillin-resistant Staphylococcus aureus (MRSA) in multi-centre Malaysian hospitals. J Hospital Infect. 2024; 143: 113-114.
[22] Shuaibu AS, Ibrahim YK, Olayinka BO, et al. Retrospective study on the prevalence of surgical wound infections in specialist hospital Sokoto-North West Nigeria. J Adv Med Pharmaceut Sci 2017; 11: 1-7.
[23] Kao CM, Fritz SA. Infection prevention-How can we prevent community transmission of CO-MRSA? Clini Microbiol Infect. https://www.sciencedirect.com/science/article/pii/S1198743X24000107 (2024, accessed 25 January 2024).
[24] Nakamura K, Hayakawa K, Tsuzuki S, et al. Clinical outcomes and epidemiological characteristics of bacteremia in the older Japanese population. J Infecti Chemother. Epub ahead of print 22 June 2023. doi: 10.1016/j.jiac.2023.06.015.