Le Infezioni in Medicina, n. 2, 248-253, 2024
doi: 10.53854/liim-3202-13
CASE REPORTS
Erythema nodosum leprosum necroticans: a case report of an atypical severe type 2 leprosy reaction and literature review
Alessandro Alfieri, Shinta Trilaksmi Dewi, Agnes Sri Siswati, Satiti Retno Pudjiati, Hardyanto Soebono
Department of Dermatology and Venereology, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
Article received 3 April 2024, accepted 8 May 2024
Corresponding author
Alessandro Alfieri
E-mail: andro.alfieri@mail.ugm.ac.id
SummaRY
Until now, leprosy remains a problem and challenge in the world because it can cause disability and morbidity in affected individuals, including problems due to the emergence of type 2 lepra reaction or erythema nodosum leprosum (ENL). The clinical picture of ENL can appear in an atypical and severe form, called ENL necroticans (ENN), which becomes a problem in diagnosis and therapy. We report a 17-year-old female with lepromatous leprosy and ENN who received therapy in the form of a combination of steroids and methotrexate. Four months after consuming this therapy, the ulcers on the patient’s body improved, leaving atrophic and hypertrophic scars. ENN’s unusual clinical presentation poses diagnostic difficulties in that its appearance does not follow the typical patterns, making it challenging to identify correctly. Furthermore, managing cases of ENN may necessitate supplementary treatment beyond steroids alone.
Keywords: Leprosy, type 2 leprosy reaction, Erythema nodosum leprosum necroticans.
INTRODUCTION
Leprosy is a chronic granulomatous infectious disease caused by Mycobacterium leprae that can lead to various clinical manifestations [1]. This disease remains a significant challenge, especially for developing and underdeveloped countries, as it can result in disability and morbidity for affected individuals, which impacts their quality of life. Another important issue that arises from this disease is the occurrence of leprosy reactions [2]. These are defined as acute inflammatory episodes which complicate the course of leprosy. Leprosy reactions can be classified into type 1 or reversal reaction, type 2 or erythema nodosum leprosum (ENL), and Lucio’s phenomenon [3]. ENL itself has been reported to occur in 15.4% of patients with lepromatous leprosy and 4.1% of patients with borderline lepromatous leprosy. In Brazil, the reported prevalence of ENL is 25%, while in India, the prevalence reaches 49.4% among patients with lepromatous leprosy [4, 5].
ENL is mediated by type III hypersensitivity reactions, which can occur before, during or after the initiation of anti-leprosy therapy [5]. The classic clinical manifestation of ENL is the presence of painful subcutaneous nodules accompanied by constitutional symptoms (fever, malaise, arthralgia and myalgia) as well as neuritis, uveitis, orchitis or involvement of other organ systems [5]. Atypical skin lesions of ENL can present as pustular, hemorrhagic, and erythema multiforme-like lesions, as well as the more severe form of necrotic ulcerative lesions or ENL necroticans [6]. The presence of these atypical forms of ENL poses new challenges in diagnosis and treatment, particularly when the atypical presentation is the initial manifestation of leprosy [3].
We report a case of a 17-year-old female with ENL necroticans in lepromatous leprosy and grade 2 disability who was undergoing multidrug therapy (MDT). This case report aims to provide an illustration of an atypical form of ENL skin lesions, thereby improving clinician knowledge and allowing early identification of this entity.
CASE ILLUSTRATION
A 17-year-old female, who had been diagnosed with lepromatous leprosy and received multibacillary (MB) multidrug therapy (MDT), came to the Dermatology and Venereology outpatient clinic of Dr. Sardjito General Hospital in Yogyakarta, Indonesia, complaining of ulcers on her body, both arms, and both legs. Three months after being diagnosed with leprosy and started consuming MDT, she complained of the emergence of painful red nodules on the extremities, which were diagnosed as ENL and treated with oral methylprednisolone (MP) 32 mg for two weeks and tapered down to 24 mg for another two weeks. When the MP was tapered down, the nodules developed into painful ulcers. In addition, the patient also experienced symptoms such as fever, joint pain, and fatigue.
On physical examination, the patient’s temperature was 38.7 °C and enlarged cervical lymph nodes were palpated. On skin examination, multiple ulcers with necrotic tissue bases were found, covered with thick black crusts of varying sizes scattered on the ears, arms, trunk, and legs (Figure 1A). Enlargement of the right and left common peroneal nerves was found, which was painful in palpation. Based on the physical examination, the differential diagnosis was ENL necroticans and Lucio’s Phenomenon in a patient with lepromatous leprosy. Laboratory examination showed leucocytosis with predominance of neutrophils. Slit skin smear from ear lobe and the skin lesion showed acid fast bacilli (AFB) with bacteriological index 5+ and morphological index 50%. Human immunodeficiency virus (HIV) and Hepatitis B tests revealed non-reactive. The swab examination from the base of the ulcers demonstrated no bacterial or fungal growth. Histopathology examination demonstrated inflammatory cells with a predominance of foamy macrophages and very few lymphocytes forming granulomas in the periappendages and perivascular areas. In the subcutaneous tissue, granulomas consisting of foamy macrophages were evident. Many blood vessels were found with extravasation of erythrocytes and fibrinoid necrosis (Figure 2A). The Fite-Faraco staining revealed scattered acid-fast bacilli with a few globi, and some were in the endothelial lumen, equal to a bacteriological index of 6+ (Figure 2B).
Based on the anamnesis, physical examination, and supporting examinations, the patient was diagnosed with lepromatous leprosy with ENL necroticans and continued for MB-MDT, as well as received an additional oral MP 32 mg for two weeks. During the two-week follow-up examination, there was no improvement, and MP 32 mg was continued for another two weeks. On the next follow-up, moon face and weight gain were evident. Therefore, MP was tapered down to 24 mg, and the patient also received a steroid-sparing agent, oral methotrexate 10 mg, for the next two weeks. After receiving this regimen, no new lesions were found, and the regimen was continued for another two weeks, from which ulcers started to dry out. Four months after consuming this therapy and tapering down the MP to 4 mg, the ulcers on the patient’s body improved, leaving hypertrophic scars (Figure 1B).

Figure 1 - (A) Ulcers with necrotic tissue bases, covered with thick black crusts of varying sizes, multiple, scattered (B) Hyperpigmented hypertrophic scars at the site of healed ulcer.
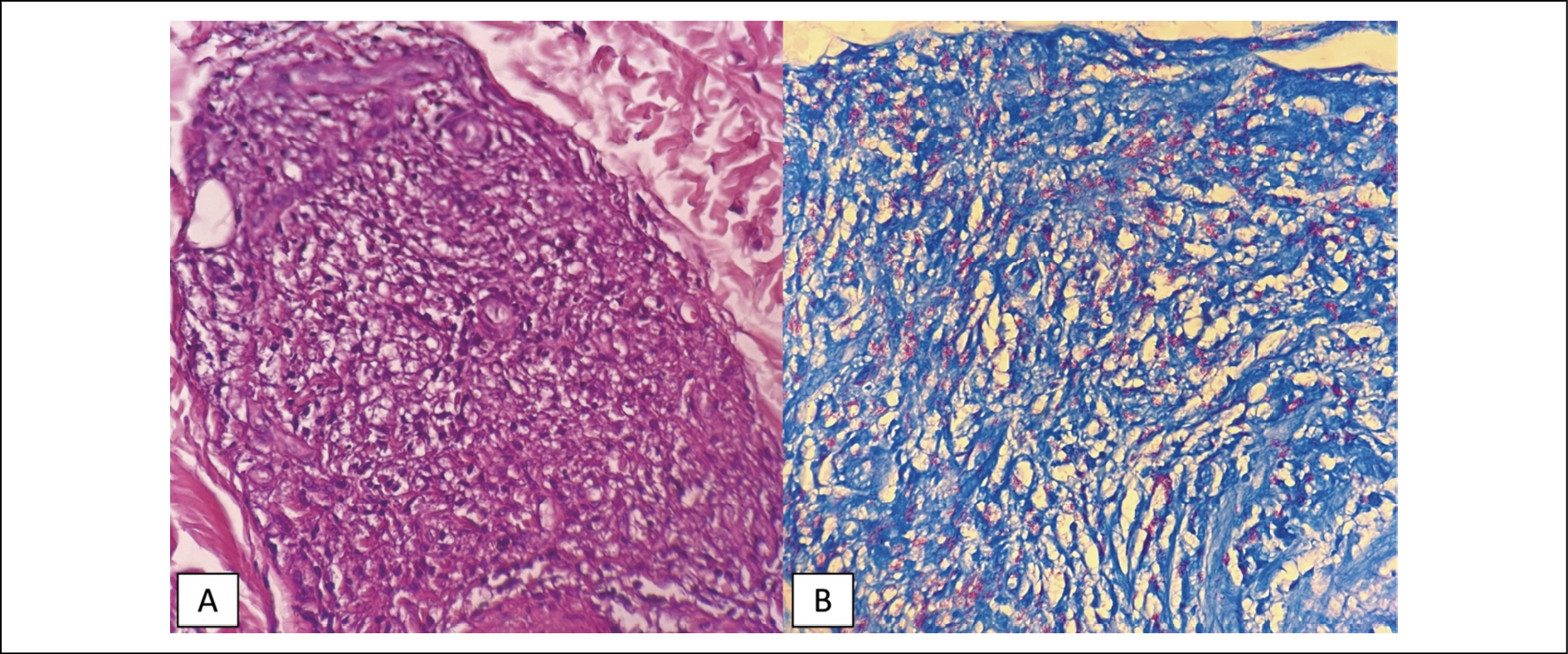
Figure 2 - (A) Hematoxylin & Eosin staining showed inflammatory cells in periappendages and perivascular, with a predominance of foamy macrophages and very few lymphocytes, forming granulomas. In subcutaneous tissue, there were also granulomas consisting of foamy macrophages. Many blood vessels were found with extravasation of erythrocytes and fibrinoid necrosis; (B) Fite-Faraco staning showed scattered acid-fast bacilli with some formed globus, and some were in the endothelial lumen.
DISCUSSION
Leprosy type II reaction or erythema nodosum leprosum (ENL) is a type III hypersensitivity reaction involving antigens, antibodies, and complements, although the exact pathomechanism is still poorly understood. Neutrophils have been reported to play an important role in the occurrence of ENL. This is evidenced by neutrophil infiltration on histopathological examination, especially during the acute phase [7]. Increased cytokines such as TNF-α and IFN-γ have also been reported to occur in ENL cases. In addition, other proinflammatory cytokines such as IL-1β, IL-4, IL-6, IL-8, IL-10, IL-12, and cytokine receptors such as sIL2R and sIL6R also play a role in the occurrence of ENL. These suggest that the use of inhibitors for these molecules may be useful in clinical settings [8].
Several risk factors have been reported for the occurrence of ENL, including patients with lepromatous leprosy (LL) type, high bacterial index, pregnancy, breastfeeding, stress, puberty, infection, vaccination, HIV, patients with malaria, and patients with tuberculosis [9]. In our case, the patient was diagnosed with LL based on the clinical examination, histopathological examination, and slit skin smear examination. Additionally, the patient was 17 years old at the time of diagnosis, which is still within the age range of puberty. Therefore, our patient had multiple risk factors for the occurrence of ENL.
ENL necroticans (ENN) is a severe clinical manifestation of ENL, which is a rare condition reported in only 8% of patients with ENL which can be characterized by vesicular, bullous or pustular lesions that necrosis and develop into ulcers [2, 10]. This condition was first reported by Verma and Pandhi in 1993 in India and could mimic other diseases, for example, Sweet’s syndrome, cutaneous vasculitis, systemic-onset juvenile idiopathic arthritis, leishmaniasis, or even malignant syphilis [11-16]. ENN usually occurs in cases of borderline lepromatous leprosy (BL) and lepromatous leprosy (LL), particularly when patients initiate MDT. The main complaints are painful ulcers, accompanied by constitutional symptoms, involvement of other organs, and neuritis [11]. Consistently, our patient had classic manifestations of ENN, consisting of painful ulcers in the ENL lesions, fever, enlargement of cervical lymph nodes, and neuritis of the right and left common peroneal nerves.
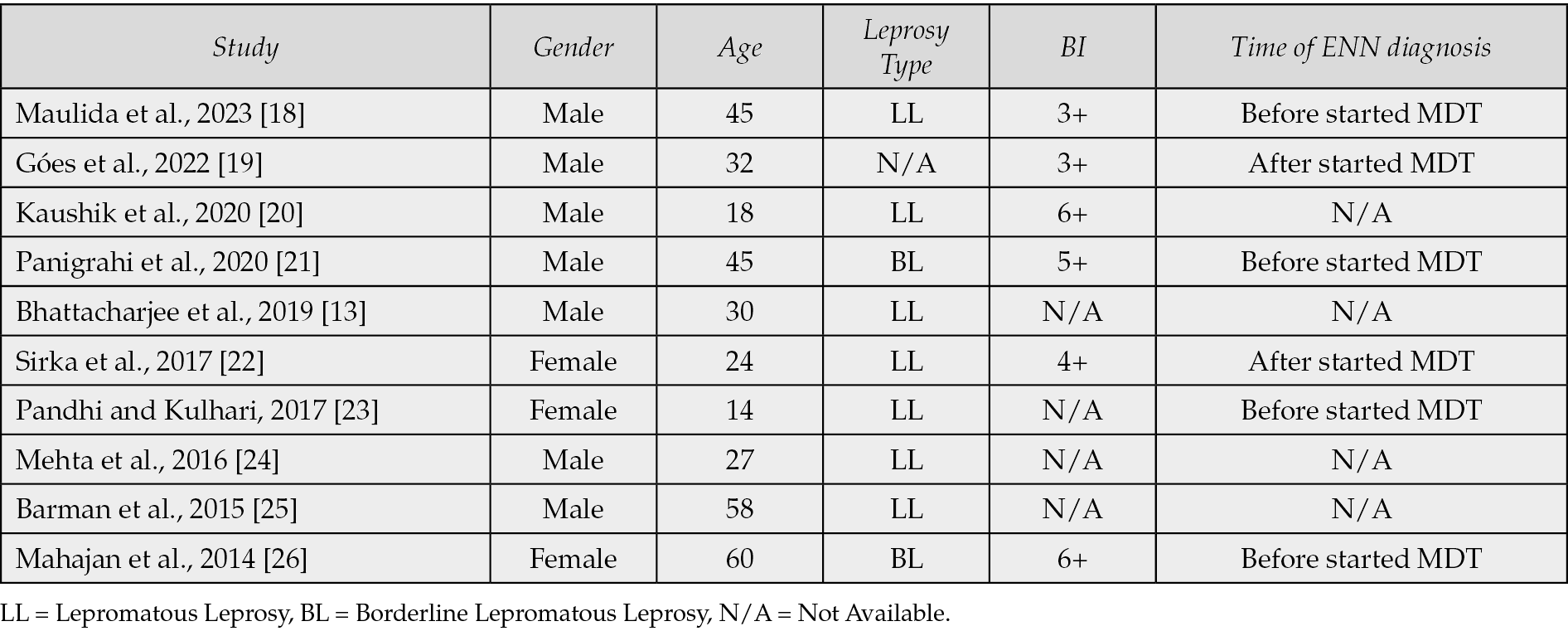
Based on a literature search via PubMed with the keywords “erythema”, “nodosum”, “leprosum”, and “necrotic” in the last ten years, eleven case reports regarding ENN were found, from which one of them was excluded due to missing full paper (Table 1). Based on the case reports, ENN occurred more frequently in males (70%) with an average age of 35.3 years. Seven cases (70%) of ENN were reported to occur in the lepromatous leprosy (LL) type, 2 cases in the borderline lepromatous (BL) type (20%), and one case did not clearly mention the leprosy type. In most cases (60%), the bacterial index was found to be ≥3+. In four cases (40%), ENN was diagnosed before the patients started MDT, and in two cases (20%), ENN was diagnosed after the patients started MDT.
Table 1 - Reported cases of erythema nodosum leprosum necroticans.
Lucio’s Phenomenon (LP) is the main differential diagnosis of ENN since it can also present with vasculonecrotic reactions [27]. LP usually occurs in cases of untreated or inadequately of non-nodular treated LL cases and most commonly develops between one to three years after the first manifestation of leprosy. The early sign of LP is the presence of painful erythematous patches or plaques in the extremities, which evolve into geometric or jagged-edge necrotic ulcers with a depth between 0.5 and 1 cm. However, no constitutional symptoms, involvement of other organs, and neuritis are found in LP [28].
The management of ENN is similar to that of classic ENL cases, with the main goals of controlling inflammation, reducing pain, and preventing severe disabilities. Corticosteroids, such as prednisone, are the first-line therapy for ENL because they can precisely control inflammation and pain. A high dose of prednisone is usually required, followed by a slow tapering according to the patient’s clinical condition. However, steroids often cause side effects when used continuously, so their use must be closely monitored [10]. In addition to steroids, thalidomide has been reported as an effective alternative therapy for ENL. Thalidomide can provide a rapid anti-inflammatory effect by inhibiting TNF-α protein synthesis. Currently, the administration of thalidomide is recommended for men and postmenopausal women because it has teratogenic effects when given to childbearing-age women, but it’s not available yet at our center [29, 30].
Methotrexate (MTX) can be used in patients who are unresponsive to the use of corticosteroids and thalidomide as a steroid-sparing agent [31]. It was also reported that MTX had good outcomes, especially for patients who had severe complications from leprosy. While the exact mechanism of action of MTX in ENL is currently unclear, it is widely recognized that MTX acts on inflammatory cytokines, such as TNF-a, IL-1, and IL-6, which contribute to the pathogenesis of ENL [32]. Nevertheless, it was reported that the outcome of MTX use was only evident after 8-12 weeks of use [33]. In this case, the addition of methotrexate was considered because the patient had already experienced side effects from the use of steroids, such as weight gain and moon face. Several studies have reported alternative therapies for ENL, such as clofazimine, pentoxifylline, cyclosporine, azathioprine, etanercept, colchicine, chloroquine, minocycline, and zinc. However, the efficacies of these drugs were still varied [10, 34].
CONCLUSIONS
Erythema nodosum leprosum necroticans (ENN) is an uncommon, atypical manifestation of type 2 lepra reaction. It can occur before, during, or after someone has undergone treatment for leprosy. ENN’s unusual clinical presentation poses diagnostic difficulties that its appearance does not follow the typical patterns, making it challenging to identify correctly. Furthermore, managing cases of ENN may necessitate supplementary treatment beyond steroids alone.
Conflicts of interest
None.
Funding
None.
Acknowledgements
A written consent was obtained from patient.
REFERENCES
[1] Benard G, Sakai-Valente NY, Bianconcini Trindade MA. Concomitant Lucio phenomenon and erythema nodosum in a leprosy patient: clues for their distinct pathogeneses. Am J Dermatopathol. 2009; 31(3): 288-292. doi:10.1097/DAD.0b013e318193c74c.
[2] Wankhade VH, Debnath P, Singh RP, Sawatkar G, Bhat DM. A retrospective study of the severe and uncommon variants of erythema nodosum leprosum at a tertiary health center in central India. Int J Mycobacteriol. 2019; 8(1): 29-34. doi:10.4103/ijmy.ijmy_174_18.
[3] Alakad R, Nofal A, Assaf M. Atypical presentations of erythema nodosum leprosum: Diagnostic and therapeutic aspects. J Dtsch Dermatol Ges. 2021; 19(8): 1133-1143. doi:10.1111/ddg.14449.
[4] Voorend CG, Post EB. A systematic review on the epidemiological data of erythema nodosum leprosum, a type 2 leprosy reaction. PLoS Negl Trop Dis. 2013; 7(10): e2440. doi:10.1371/journal.pntd.0002440.
[5] Singal A. Current Concepts and Challenges in the management of erythema nodosum leprosum. Indian Dermatol Online J. 2020; 11(4): 479-481. doi: 10.4103/idoj.IDOJ_69_20.
[6] Dhillon K, Sharma D, Singh T, et al. Erythema necroticans: a rare reaction pattern in leprosy. Int J Adv Med. 2015; 2(2): 185-187.
[7] Schmitz V, Tavares IF, Pignataro P, et al. Neutrophils in Leprosy. Front Immunol. 2019; 10: 495. doi: 10.3389/fimmu.2019.00495.
[8] Polycarpou A, Walker SL, Lockwood DN. A Systematic Review of Immunological Studies of Erythema Nodosum Leprosum. Front Immunol. 2017; 8: 233. doi:10.3389/fimmu.2017.00233.
[9] Sharma N, Koranne RV, Mendiratta V, Sharma RC. A study of leprosy reactions in a tertiary hospital in Delhi. J Dermatol. 2004; 31(11): 898-903. doi:10.1111/j.1346-8138. 2004.tb00623.x.
[10] Bhat RM, Vaidya TP. What is New in the pathogenesis and management of erythema nodosum leprosum. Indian Dermatol Online J. 2020; 11(4): 482-492. doi: 10.4103/idoj.IDOJ_561_19.
[11] Verma KK, Pandhi RK. Necrotic erythema nodosum leprosum; a presenting manifestation of lepromatous leprosy. Int J Lepr Other Mycobact Dis.1993; 61(2): 293-294.
[12] Heng YK, Chiam YT, Giam YC, Chong WS. Lepromatous leprosy in erythema nodosum leprosum reaction mimicking Sweet’s syndrome. Int J Dermatol. 2011; 50(9): 1124-1125. doi: 10.1111/j.1365-4632.2010.04686.x.
[13] Bhattacharjee R, Chatterjee D, Narang T, Dogra S. Necrotic erythema nodosum leprosum masquerading as cutaneous vasculitis. Rheumatology (Oxford). 2019; 58(1): 85. doi:10.1093/rheumatology/key216.
[14] Pradhan S, Prasad Nayak B, Padhi T, Sethy M. Bullous Erythema Nodosum Leprosum masquerading as systemic onset juvenile idiopathic arthritis: A case report. Lepr Rev. 2015; 86(4): 387-390.
[15] Dagenet CB, Davis MS, Murphy S, Thiede R, Culpepper KS, Fazel M. Limited cutaneous leishmaniasis as ulcerated verrucous plaque on leg, Tucson, Arizona, USA1. Emerg Infect Dis. 2023; 29(6): 1268-1269. doi: 10.3201/eid2906.230125.
[16] Li JH, Guo H, Gao XH, Chen HD. Multiple skin ulcers from malignant syphilis. Lancet. 2015; 386(10003): 1564. doi:10.1016/S0140-6736(15)60157-X
[17] Galeano J, Contreras A, Pabón L, Ruiz AC, Serrano-Coll H, Arboleda M. Case report: necrotizing erythema nodosum as a manifestation of lepromatous leprosy relapse 50 years after the initial infection. Am J Trop Med Hyg. 2023; 109(1): 53-56. doi: 10.4269/ajtmh.22-0701.
[18] Maulida M, Vella V, Budini SS, et al. Systemic manifestation of necrotic erythema nodosum leprosum: A case report of a fatal leprosy. Narra J. 2023; 3(2): e216. doi: 10.52225/narra.v3i2.216.
[19] Góes LDM, Morais PM, Rebello PFB, Schettini APM. Necrotic erythema nodosum reaction associated with histological alterations of Lucio’s phenomenon. An Bras Dermatol. 2022 Mar-Apr; 97(2): 231-235. doi: 10.1016/j.abd.2020.09.016.
[20] Kaushik A, Dogra S, Narang T. Lichenoid skin nodules as presenting feature of necrotic erythema nodosum leprosum in leprosy. Am J Trop Med Hyg. 2020; 103(1): 9. doi: 10.4269/ajtmh.20-0177.
[21] Panigrahi A, Sil A, Bhanja DB. Erythema necroticans. QJM. 2020; 113(9): 685-686. doi: 10.1093/qjmed/hcz323.
[22] Sirka CS, Panda M, Pradhan S, Baisakh MR. Necrotic Erythema Nodosum Leprosum Healing with Extensive Scars. Indian Dermatol Online J. 2017; 8(6): 509-511. doi: 10.4103/idoj.IDOJ_39_17.
[23] Pandhi D, Kulhari A. Erythema nodosum leprosum necroticans. Indian Pediatr. 2017; 54(12): 1071. doi: 10.1007/s13312-017-1218-8.
[24] Mehta N, Ramachandran R, Srikanth S. Erythema Necroticans - A Case Report. Indian J Lepr. 2016; 87(4): 255-257.
[25] Barman KD, Madan A, Garg VK, Goel K, Khurana N. Unusual presentation of necrotic erythema nodosum leprosum on scalp: a case report. Indian J Lepr. 2015; 87(1): 23-26.
[26] Mahajan VK, Abhinav C, Mehta KS, Chauhan PS. Erythema nodosum leprosum mimicking Sweet’s syndrome: an uncommon presentation. Lepr Rev. 2014; 85(4): 322-327.
[27] Fogagnolo L, de Souza EM, Cintra ML, Velho PE. Vasculonecrotic reactions in leprosy. Braz J Infect Dis. 2007; 11(3): 378-382. doi:10.1590/s1413-86702007000300016.
[28] Ranugha P, Chandrashekar L, Kumari R, Thappa DM, Badhe B. Is it Lucio phenomenon or necrotic erythema nodosum leprosum? Indian J Dermatol. 2013 Mar; 58(2): 160. doi: 10.4103/0019-5154.108087.
[29] Mahmoud M & Walker S. A systematic review of adverse drug reactions associated with Thalidomide in the treatment of Erythema Nodosum Leprosum. Lepr Rev. 2019; 90: 42-60.
[30] World Health Organization. Expert committee on leprosy. Eight Report. World Health Organ Tech Rep Ser. 2012; 968: 1-61.
[31] de Barros B, Lambert SM, Shah M, et al. Methotrexate and prednisolone study in erythema nodosum leprosum (MaPs in ENL) protocol: a double-blind randomized clinical trial. BMJ Open. 2020; 10(11): e037700. doi: 10.1136/bmjopen-2020-037700.
[32] Bedoui Y, Guillot X, Sélambarom J, et al. Methotrexate an old drug with new tricks. Int J Mol Sci. 2019; 20(20): 5023. doi: 10.3390/ijms20205023.
[33] Mehta H, Narang T, Dogra S, Kumar B. Methotrexate in erythema nodosum leprosum: Pitfalls to avoid. Trop Doct. 2022; 52(1): 226-227. doi: 10.1177/00494755211056170.
[34] Rani S, Singh S, Agrawal D, Sardana K, Ahuja A. An uncommon variant of erythema nodosum leprosum responding well to methotrexate: Report of two cases. Trop Doct. 2021; 51(4): 569-572. doi:10.1177/00494755211016652.