Le Infezioni in Medicina, n. 3, 412-417, 2022
doi: 10.53854/liim-3003-9
ORIGINAL ARTICLES
Home management of COVID-19 symptomatic patients: a safety study on COVID committed home medical teams
Sergio Venturini1, Daniele Orso2, Francesco Cugini3, Francesco Martin4, Cecilia Boccato4, Laura De Santi5, Elisa Pontoni5, Silvia Tomasella5, Fabrizio Nicotra5, Alessandro Grembiale6, Maurizio Tonizzo6, Silvia Grazioli6, Sara Fossati1, Astrid Callegari1, Giovanni del Fabro1, Massimo Crapis1
1Department of Infectious Diseases, ASFO “Santa Maria degli Angeli” Hospital of Pordenone, Italy;
2Department of Anesthesia and Intensive Care, ASUFC “Santa Maria della Misericordia” University Hospital
of Udine, Italy;
3Department of Emergency Medicine, ASUFC Hospital of San Daniele, Udine, Italy;
4Committed Home Medical Teams, ASFO “Santa Maria degli Angeli” Hospital of Pordenone, Italy;
5Department of Emergency Medicine, ASFO “Santa Maria degli Angeli” Hospital of Pordenone, Italy;
6Department of Medicine, ASFO “Santa Maria degli Angeli” Hospital of Pordenone, Italy
Article received 9 April 2022, accepted 7 June 2022
Corresponding author
Daniele Orso
E-mail: sd7782.do@gmail.com
SummaRY
To reduce the overburden in the hospital, during the COVID-19 pandemic, some “COVID Committed Home Medical Teams” (CCHTs) were created in Italy. These units consist of a small pool of general practitioners who aim to evaluate all patients with COVID-19 who require a medical examination directly at home. After the first visit (which can end with patient hospitalisation or home management), CCHTs periodically monitor the patients’ clinical conditions and vital signs (usually a revaluation every 24-48 hours, except for a sudden worsening). However, this strategy - which reduces the pressure on hospitals - has never been evaluated for patient safety. Our study aims to determine whether a home-based monitoring and treatment strategy for non-severe COVID-19 patients was safe as direct hospital admission by the emergency department. We conducted a retrospective observational study about 1,182 patients admitted to the hospital for COVID-19 between September 2020 and April 2021, confronting in-hospital and 30-day mortality in both CCHT-referred (n=275) and directly admitted by emergency department (n=907). Patients assessed by the CCHT had lower in-hospital and 30-day mortality (18% vs 28%, p=0.001; and 20% vs 30%, p=0.002); but, in the propensity score matching comparison, there was no characteristic between the two groups turned out significantly different. CCHT did not correlate with in-hospital or 30-day mortality. CCHT is a safe strategy to reduce hospital overburden for COVID-19 during pandemic surges.
Keywords: COVID-19, SARS-CoV-2, home management, mortality.
INTRODUCTION
The outbreak of COVID-19 caused by SARS-CoV-2 poses a serious challenge to the healthcare system’s resilience around the world. As many healthcare systems have spent most of their resources on COVID-19, they need to use resources outside the hospital to relieve and avoid collapse [1]. In particular, hospital capacity and availability of beds and ventilators were identified among the highest relevant factors, which were critically exceeded in many countries during the pandemic.
If globally considered, approximately 81% of patients with COVID-19 present mild disease, typically reflected in oxygen saturation of 90% or above. This subpopulation of patients may not require inpatient hospitalization and could benefit from at-home oxygen supplementation and monitoring [2]. Health systems facing the challenge of the COVID-19 pandemic need to explore further opportunities by ensuring, for example, the management of home care. This latter strategy could reduce the burden on the health system and increase capacity for severe cases during surges. However, the risk of hospitalization should not be ignored; therefore, frequent and efficient monitoring is essential. The decision to shift the patient to an inpatient setup should be based on the clinical presentation and potential risk factors for severe disease. Patients at high risk of progression for severe illness should be monitored closely. Some “COVID Committed Home Medical Teams” (CCHTs, in Italy named USCA, Unità Speciali di Continuità Assistenziale) were created for this reason in Italy. These units consist in a small pool of general practitioners who have the primary aim of evaluating all COVID-19 patients who require a medical examination. Every team was equipped with a sthetoscope, a pulsoxymeter and a portable ultrasound. After the first visit (which can end with patient hospitalisation or home management), CCHTs periodically monitor the patients’ clinical conditions and vital signs (usually a revaluation every 24-48 hours, except for a sudden worsening).
However, this strategy - which reduces the pressure on hospitals - has never been evaluated for patient safety. Our study aims to verify the safety of home management patients suffering from COVID-19.
PATIENTS AND METHODS
Study protocol
This study was a retrospective observational study of prospectively and systematically collected data about all patients with SARS-CoV-2 admitted and recovered to Pordenone Hospital, Italy, from September 21, 2020, to April 30, 2021. The patient’s consent was obtained through the general consent system, and the European General Data Protection Regulation 2016/679 was respected.
Study population
Inclusion criteria were: patients admitted to the Pordenone hospital with a positive nasopharyngeal molecular or antigenic swab test, patients with >18 years of age.
Exclusion criteria were: pregnancy, pediatric patients, refusal of consent.
Recorded data
Patient outcomes were recorded in terms of in-hospital mortality and at 30-days of follow-up. Clinical parameters such as age, gender, and any comorbidity from medical history and clinical conditions at admission were recorded. Arterial blood gas analysis at the first evaluation was also recorded. Disease severity scores such as NEWS and ROX were also recorded.
Study outcome
The main aim was to verify if the COVID-19 patients referred to the ED by the CCHT and admitted to the hospital had statistically different in-hospital and 30-day mortality compared to COVID-19 patients not assessed by the CCHT.
The secondary aim was to evaluate the correlation between the recorded variables - including the evaluation by the CCHT - and the outcomes considered.
Statistical analysis
The distribution between the two groups was compared by Mann-Whitney test (variables are expressed as a median and inter-quartile range) after verifying the normality of the distribution employing the Shapiro-Wilk test. In contrast, Fisher’s exact test (or Pearson test) was used for variables expressed as absolute frequency and relative percentage. We also verified the correlation between the measured variables and the outcome by stepwise generalised linear regression analysis. A p-value <0.05 was considered statistically significant.
All statistical analyses were performed using open-source software “R: A language and environment for statistical computing”, implementing the “readODS”, “compareGroups”, “ggplot2” packages.
RESULTS
During the study period, 2,821 patients were visited at least once by the CCHT. In the same period, 1,182 patients were evaluated for COVID-19 in Pordenone Hospital ED at least once and admitted. Of these, 275 were referred to the ED by the CCHT.
The clinical characteristics of the two groups of patients are described in Table 1. The two groups of patients are comparable in age, sex and comorbidity. The arterial blood gas analysis values were also overlapping. At the unmatched analysis, patients assessed by the CCHT had a lower in-hospital and 30-day mortality (respectively 18% vs 28%, p=0.001; and 20% vs 30%, p=0.002). Patients evaluated by the CCHT most frequently presented with at least one febrile episode at assessment (48% vs 27%, p<0.001) and a positive 6-minutes walking test (17% vs 12%, p=0.02). However, in the propensity score matching comparison, no characteristic between the two groups turned out significantly different.
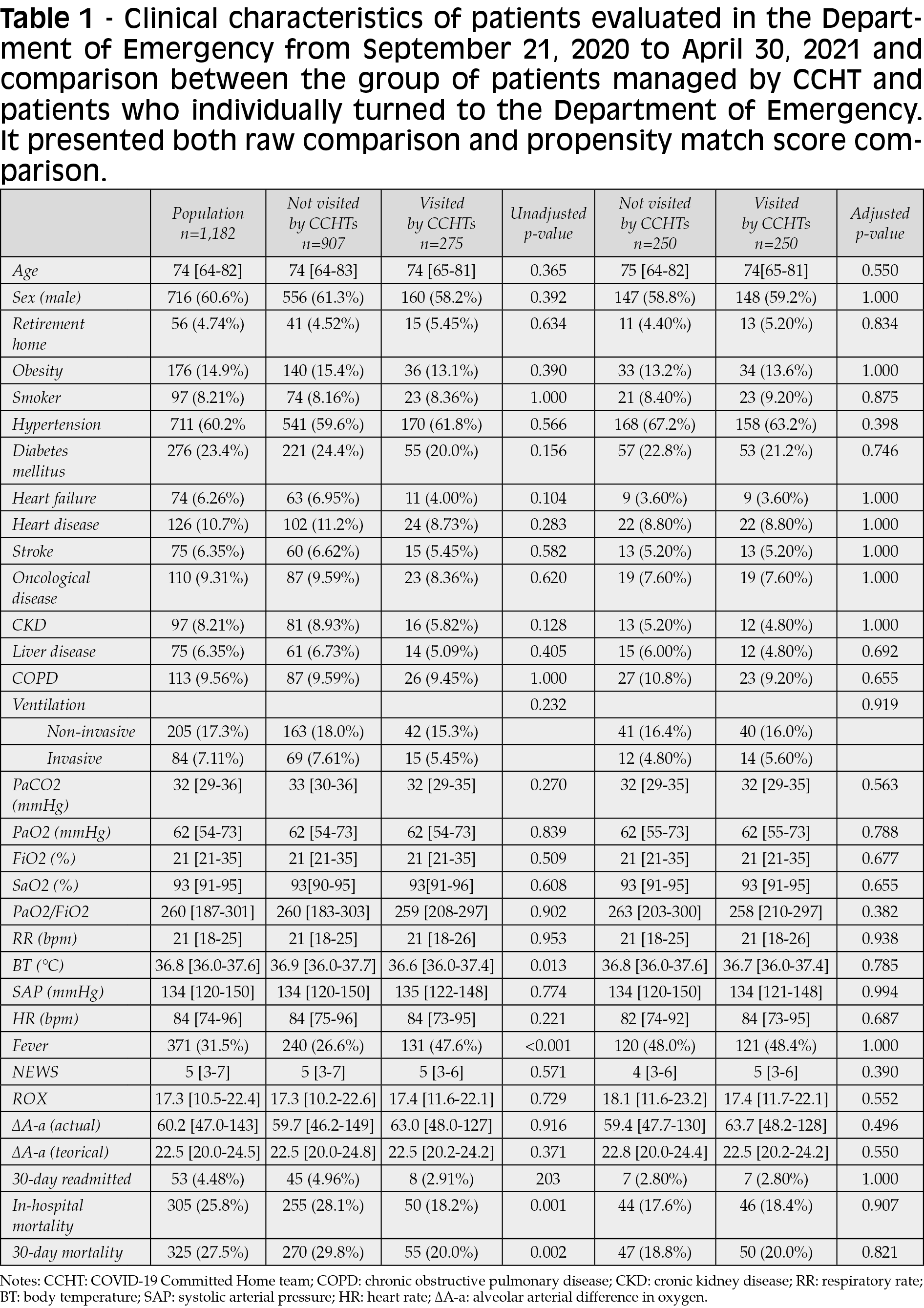
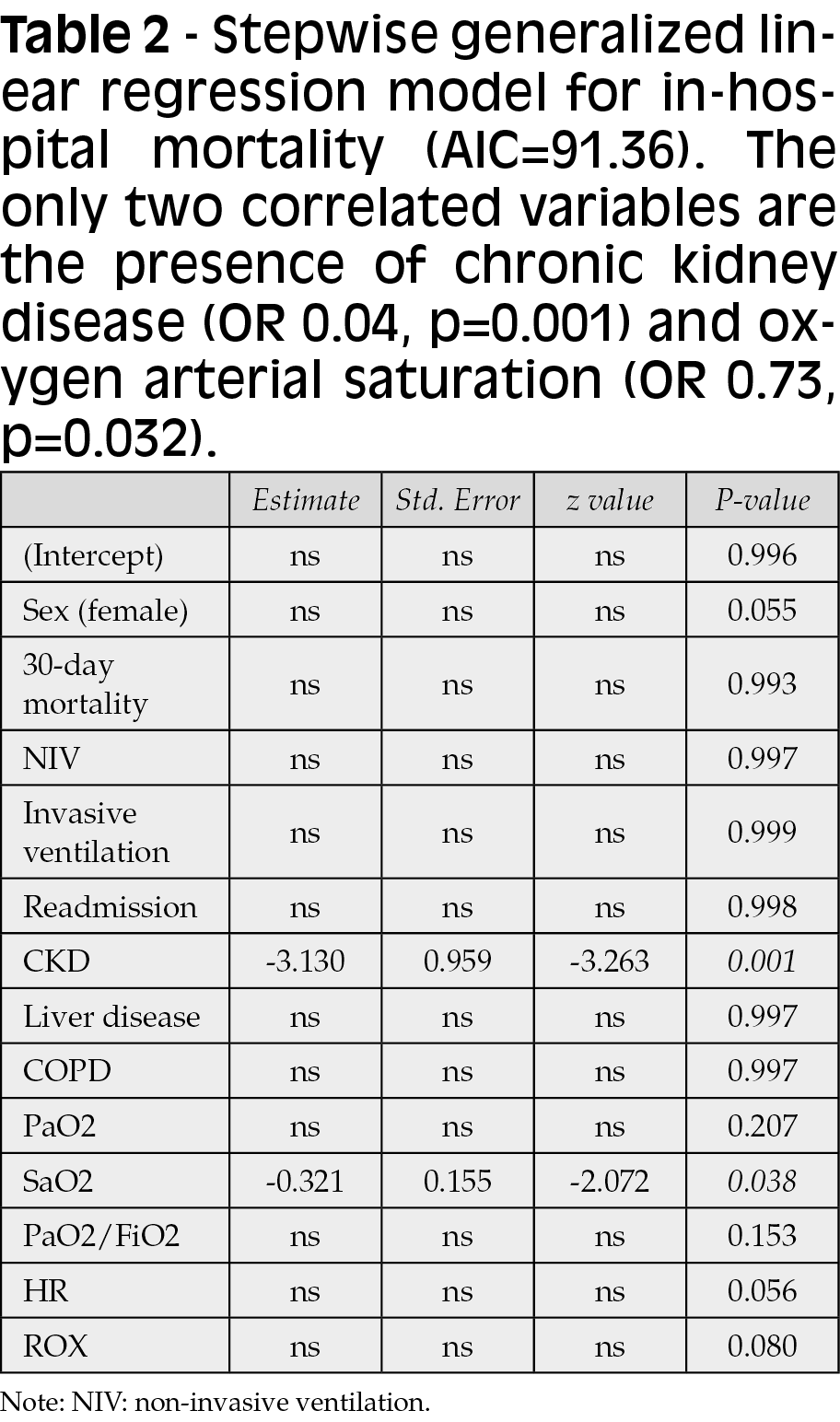
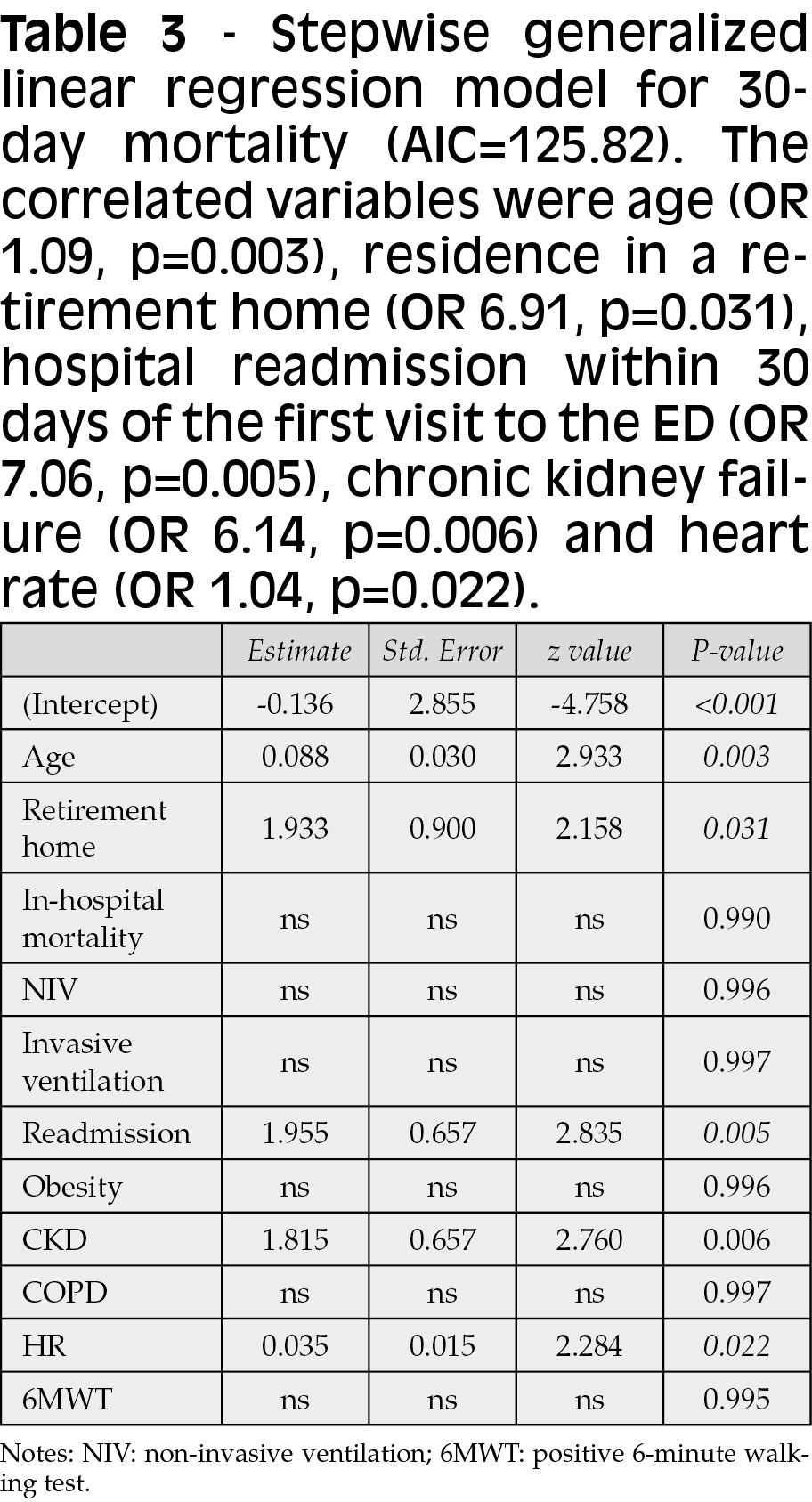
At the stepwise generalized linear regression analysis, the factors related (inverse correlation) to death during hospitalization (AIC 91.36) were chronic kidney failure (OR 0.04, p=0.001) and arterial oxygen saturation value (OR 0.73, p=0.032) (Table 2). For the 30-day mortality regression model (AIC 125.82), the correlated variables were age (OR 1.09, p=0.003), residence in a retirement home (OR 6.91, p=0.031), hospital readmission within 30 days of the first visit to the ED (OR 7.06, p=0.005), chronic kidney failure (OR 6.14, p=0.006) and heart rate (OR 1.04, p=0.022) (Table 3).
DISCUSSION
Our study shows that CCHT-based management of symptomatic but non-severe COVID-19 patients is safe, resulting in a remarkably low number (around 10%) of patients addressed to the hospital. This strategy could better optimise the limited resources available during a pandemic [3]. This approach saves hospital resources to be reserved for a limited number of patients who can be identified safely with low-level medical evaluation. Hospital overcrowding during major pandemic surges is responsible for a - at least indirect - mortality rate from COVID-19 [4, 5]. In industrialised countries, the overload of hospital health systems is a scenario that pushes the entire system to the brink of collapse if an unpredictable mass event such as a pandemic occurs [6]. The ability to manage (detect, monitor and select patients at greater risk) patients with COVID-19 at home has a double value: on one hand, it reduces the pressure on hospitals. On the other hand, it could allow, at least theoretically, a reduction in the spread of the disease by reducing interpersonal contact in crowded environments [7]. In fact, only a small percentage of patients with COVID-19 require hospitalization [8]. However, the widespread of the disease accounts for the huge overload of patients in a short time during epidemic peaks. Similar experiences, such as that of Dirkgil et al. and Grutters et al., have shown that home management through telemedicine is feasible and reduces the number of accesses to the Eds [9, 10]. Nonetheless, these studies are concerned with shortening hospital length of stay through post-discharge monitoring. Our practise differs from theirs in managing patients at home before turning to the ED, allowing triage even before the patient needed hospitalisation by monitoring disease progression and severity. In addition, our experience shows that mortality - both intra-hospital and the 30-day - is not increased by such a home management strategy.
Our results, in line with the literature [16], show that arterial saturation in oxygen is a short-term mortality directly related parameter of COVID-19 patients [11-14]. This strategy could permit that, with an easily feasible and low-cost test, it is possible to determine the severity and the risk class to which the patient belongs, at least in terms of screening, to direct the patient to the hospital [15]. As some studies have suggested, widespread SpO2 self-monitoring at home (at rest and after walking test) in non-severe COVID-19 could be crucial, reserving anothers testing (blood count, CPR, DDimer, chest X-ray or TC scan) to a more severe disease stage [16, 17].
Our study suggests that patients with chronic renal failure are a particularly at-risk subpopulation. In fact, given the apparent protective role of this pathology in intra-hospital mortality, conversely, it turns out to be a negative prognostic factor concerning mortality at 30 days. Unfortunately we cannot establish the inverse correlation of chronic renal disease with intra-hospital mortality (identified early as patients at high risk and therefore subjected to more intensive treatment?). What also emerges from the literature is that these patients are probably a particularly frailty population, and the mortality at 30 days could be linked to the basic conditions rather than to the respiratory failure induced by COVID-19 [18].
Whether these patients should be addressed to hospital care early or be managed at home will need to be investigated in future targeted studies. Overall, we can infer that these patients seem to have been properly managed, at least in the initial stages, considering the intra-hospital mortality figure.
Ultimately, the home management of COVID-19 patients via CCHTs is a strategy that reduces the number of hospital admissions and is also safe by not burdening the mortality of these patients.
Limitations
Although similar teams for the home management of COVID-19 patients have been organised throughout Italy, we cannot claim that our experience is generalisable. Ours was a retrospective single-centre observational study, and thus, results may not be widely generalisable. Other factors, such as the relationship between general practitioners and patients, could play a significant role.
Although we closely followed ED-admitted patients, we could not trace all long-term data of COVID-19 patients not managed by CCHT and not presented in the ED. This limit is difficult to get around, considering that many patients do not have severe symptoms and do not require advanced monitoring. However, we have cross-checked the demographic data, and there is no excessive extra-hospital mortality compared to a similar period in the territory concerned.
Finally, for the design of our study, we cannot establish the reason for the readmission within 30 days of COVID-19 patients. However, while it may be linked to an erroneous assessment by CCHT or the ED’s staff, 30-day mortality is in line with existing literature, demonstrating effective patient monitoring even at home [19].
CONCLUSIONS
The CCHTs are a safe strategy to reduce hospital overburden for COVID-19 during pandemic surges without aggravating the mortality of patients.
Competing interests
No conflict of interest must be declared for any of the authors.
Funding
No fund was used for this study.
REFERENCES
[1] WHO. Strengthening the health system response to COVID-19. In: WHO/Health topicd [website]. Copenhagen: WHO Regional Office for Europe; 2020.
[2] The novel coronavirus pneumonia emergency response epidemiology team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus disease - China, 2020. China CDC Weekly. 2020; 2, 113-22.
[3] Borgen I, Romney MC, Redwood N, et al. From hospital to home: an intensive transitional care management intervention for patients with COVID-19. Popul Health Manag. 2021; 24 (1), 27-34.
[4] Routsi C, Magira E, Kokkoris S, et al. Hospital resources may be an important aspect of mortality rate among critically ill patients with COVID-19: the paradigm of Greece. J Clin Med. 2020; 9 (11), 3730.
[5] Block BL, Smith AK, Sudore RL. During COVID-19, outpatient advance care planning is imperative: We need all hands on deck. J Am Geriatr Soc. 2020; 68 (7), 1395-7.
[6] Mareiniss DP. The impending storm: COVID-19, pandemics and our overwhelmed emergency departments. Am J Emerg Med. 2020; 38 (6): 1293-4.
[7] Lukas H, Xu C, Yu Y, Gao W. Emerging telemedicine tools for remote COVID-19 diagnosis, monitoring, and management. ACS Nano. 2020; 14 (12), 16180-93.
[8] Menachemi N, Dixon BE, Wools-Kaloustian KK, Yiannoutsos CT, Halverson PK. How many SARS-CoV-2-infected people require hospitalization? Using random sample testing to better inform preparedness efforts. J Public Health Manag Pract. 2021; 27 (3), 246-50.
[9] Dirikgil E, Roos R, Groeneveld GH, et al. Home monitoring reduced short stay admissions in suspected COVID-19 patients: COVID-box project. Eur Respir J. 2021; 58 (2), 2100636.
[10] Grutters LA, Majoor KI, Pol-Mattern ESK, Hardeman JA, van Swol CFP, Vorselaars ADM. Home-monitoring reduces hospital stay for COVID-19 patients. Eur Respir J. 2021; 58(5), 2101871.
[11] ejía F, Medina C, Cornejo E, et al. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLoS One. 2020; 15 (12), e0244171.
[12] Choi KJ, Hong HL, Kim EJ. The association between mortality and the oxygen saturation and fraction of inhaled oxygen in patients requiring oxygen therapy due to COVID-19-associated pneumonia. Tuberc Respir Dis (Seoul). 2021; 84 (2), 125-33.
[13] Chatterjee NA, Jensen PN, Harris AW, et al. Admission respiratory status predicts mortality in COVID-19. Influenza Other Respir Viruses. 2021; 15 (5), 569-72.
[14] Xie J, Covassin N, Fan Z, et al. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc. 2020; 95 (6), 1138-47.
[15] Ambreen A, Ashfaq T, Andrades M, Akhtar F, Badiuzzaman S, Baig L. General practitioner’s (GP) home management guidelines for COVID-19 patients: Guidelines. J Pak Med Assoc. 2021; 71 (3), 982-89.
[16] Greenhalgh T, Knight M, Inada-Kim M, Fulop N, Leach J, Vindola-Padros C. Remote management of covid-19 using home pulse oximetry and virtual ward suopport. Brit Med J. 2021; 372, 677.
[17] Venturini S, Pontoni E, Carnelos R, et al. Development and validation of the acute pneumonia early assessment score for safely discharging low-risk SARS-CoV-2-infected patients from the emergency department. J Clin Med. 2022; 11 (3), 881.
[18] Venturini S, Orso D, Cugini F, et al. Classification and analysis of outcome predictors in non-critically ill COVID-19 patients. Intern Med J. 2021; 51 (4), 506-14.
[19] Nersesjan V, Amiri M, Christensen HK, Benros ME, Kondziella D. Thirty-day mortality and morbidity in COVID-19 positive vs. COVID-19 negative individuals and vs. individuals tested for influenza A/B: A Population-Based Study. Front Med (Lausanne). 2020; 7, 598272.