Le Infezioni in Medicina, n. 3, 464-468, 2022
doi: 10.53854/liim-3003-17
THE INFECTIONS IN THE HISTORY OF MEDICINE
The Manchurian pandemic of pneumonic plague (1910-1911)
Spyros N. Michaleas1, Konstantinos Laios1, Marianna Karamanou1, Nikolaos V. Sipsas2, Georges Androutsos3
1Department of History of Medicine and Medical Ethics, Medical School, National and Kapodistrian University of Athens, Athens, Greece;
2Department of Pathophysiology, Medical School, National and Kapodistrian University of Athens, Athens Greece;
3Biomedical Research Foundation, Academy of Athens, Athens, Greece
Article received 31 August 2021, accepted 7 June 2022
Corresponding author
Spyros N. Michaleas
E-mail: sp.michaleas@gmail.com
SummaRY
China’s winter of 1910-1911 was one of its most difficult. A deadly airborne pneumonic plague, believed to have originated from tarbagan marmots, broke out in October 1910 in a northeastern Chinese province commonly known by the exonym Manchuria. The disease had a near 100 percent mortality rate, affecting mainly the lower socio-economic classes and eventually killing more than 60,000 people over six months. By April 1911, the epidemic was suppressed, in large part due to the efforts of a Western-educated Chinese physician, Wu Lian-Teh. Similar to the recent COVID-19 pandemic, the Great Manchurian Plague outbreak highlighted the importance of personal protective equipment, such as face masks, and a quick and efficient international medical response.
Keywords: China, Manzhouli, Harbin, Wu Lien-Teh, Mukden Conference, tarabagan marmot.
INTRODUCTION
Plague outbreaks have caused fear, despair, and social disorder throughout history. In 1910, 110 years before the recent coronavirus pandemic outbreak started in Wuhan, China, the country experienced a similar outbreak of lung disease. The Great Manchurian Plague killed more than 60,000 people, mostly in the northeastern Chinese province commonly known by the exonym Manchuria. Efforts to control the spread were similar to those taken in 2020 against COVID-19: quarantines, travel restrictions, personal protective equipment and mandatory mask wearing, and a multinational healthcare response (Figure 1) [1-4].

Figure 1 - The personal protection equipment worn during the 1911 plague epidemic in Manchuria. Credits: Institut Pasteur/Archives Henri Mollaret.
In 1905, with the help of U.S. President Theodore Roosevelt (1858-1919), the Treaty of Portsmouth formally ended the Russian-Japanese War over expansion into Manchuria. Nevertheless, by 1910, northeastern China was in the last years of the Qing Dynasty (1644-1912) and remained in a state of political unrest. Although officially under the control of China, the region’s railroad systems connected China with Russia and Japan, and all three powers continued to compete for control over the region’s resources [4]. The Treaty of Portsmouth permitted each nation to maintain a certain number of soldiers in the region for protection from thieves and for railroad administration in urban settlements.
The railway system also was divided among the three empires. The Chinese Eastern Railway, which crossed Manchuria from west to east as part of the Trans-Siberian Railway from Moscow to Vladivostok, was under Russian control, as was the area from Harbin to Ch’ang-ch’un. The Imperial Chinese Railway ran from Mukden (now Shenyang) to Peking (now Beijing) and was dominated by the Chinese government. The South Manchuria Railway began in Ch’angch’un and traveled to Mukden and Dalian, including Antung along the Korean border, and it was under Japanese control [4-7]. All three nations had military and civil power over their territories. When the plague broke out, each initiated appropriate measures to stop the outbreak and protect their interests in the region [4].
Identified in 1894 by Alexandre Yersin (1863-1943), a French-Swiss bacteriologist and physician from the Pasteur Institute, Yersinia pestis (plague) is a contagious disease that can infect both humans and animals. Interestingly, just days before Yersin, another bacteriologist, Shibasaburo Kitasato (1853-1931), also isolated the bacterium during a Hong Kong outbreak in 1984. Kitasato studied under Robert Koch (1843-1910), who discovered the agents responsible for tuberculosis, cholera, and anthrax, but his initial reports on the Yersinia pestis bacterium were rejected due to concerns about sample contamination and inaccuracy [2, 4, 6, 8, 9].
Plague has two clinical types, bubonic and pneumonic, depending on the route of infection. The most common, bubonic plague, is transmitted by the bite of an infected flea. It is characterized by swollen lymph nodes, or buboes (bubo in Latin, βουβῶν in ancient Greek), particularly in the groin and armpits. Bubonic plague causes fever, weakness, and headache within one to seven days after exposure [10]. Pneumonic plague is more toxic. It infects the lung tissues within 24 hours of exposure and can be transmitted from human to human via droplets. Pneumonic plague is likely fatal if not treated in time. A characteristic symptom of this disease is bloody cough [4-7, 10, 11].
Several major plague outbreaks have occurred around the world in the last two millennia. In the 6th century, the Plague of Justinian is believed to have started in Central Africa and then spread to the Mediterranean through Egypt. In the 14th century, The Black Death broke out in Central Asia and spread to the ports of Crimea, invading North Africa and then Europe. The Plague of London devastated England in 1665. Another outbreak started in Yunnan, China, in the 19th century, reaching Hong Kong in 1894 [4, 12]. More recently, India experienced an outbreak in 1994 [4]. Overall, more than 200 million people have died from the plague throughout the centuries [12].
Many of these diseases have zoonotic origins. For example, although not bacterial, the virus responsible for COVID-19, SARS-CoV-2, is believed to have originated in bats. Transmission from animal to human thus may have occurred via consumption of game and other wild meat products [2,13]. As previously mentioned, the bubonic plague is transmitted by the bite of an infected flea. The plague in Manchuria likely originated from the tarbagan marmot, a burrowing groundhog-like animal that was hunted for its fur (Figure 2) [1, 2, 4].

Figure 2 - Tarbagan marmot.
The Great Manchurian Plague
The Great Manchurian Plague started in northeastern China in autumn 1910. The first case occurred in Manzhouli, a town in Heilongjiang province in Inner Mongolia. At the time of the outbreak, Manzhouli was close to the Chinese-Russian border and near the Chinese Eastern Railway. On 27 October 1910, cases were identified in nearby Harbin, also in Heilongjiang province. Harbin was a sparsely populated agricultural region situated near all three railroad systems. Although mostly governed by China, the port area of Dalian was under Japanese rule. Harbin also hosted many Russians who worked for the China Eastern Railway, as well as Japanese, European, and American traders [1, 4-7].
The local marmot trade expanded rapidly when the German chemical industry developed new dyes that could transform cheap marmot fur into imitation mink, otter, and sable fur [4]. Huge numbers of migrant hunters arrived in Manchuria. However, unlike the local hunters, these inexperienced hunters often trapped and handled infected marmots, thereby exposing themselves and other hunters to disease. Crowded and unsanitary living conditions among the lower socio-economical classes exacerbated the spread. However, transmission seemed to be limited to close contact. Aside from physicians and medical staff, very few other foreigners fell ill [1, 2, 4-6, 11, 12, 14]. After an incubation period of two to five days, symptoms started with a cold sensation, loss of appetite, headache, augmented pulse rate and fever, followed by bloody cough and dyspnea within the first 24 hours of symptom onset. Pulmonary septicemia was the most common official cause of death [14].
By January 1911, more than 10,000 deaths had been recorded in Manzhouli, Harbin, Mukden, and Ch’angch’un, with very few survivors and up to 150 daily recorded deaths. The disease soon expanded to the capital city, Peking (now Beijing), infecting approximately 2.25 per 1,000 people. The crowded conditions of tarbagan marmot hunters may have exacerbated spread of the plague, as they slept close together in shared huts. Manchuria’s railway network also contributed to the rapid transmission of the disease as thousands of migrant workers returned to their homes for the New Year Festival [1, 4, 5].
Recognizing the need for protective measures
The medical response to the outbreak was rapid. Russia established a makeshift plague hospital and observation site for suspected plague in the Moscow barracks of Harbin [2, 4, 5]. Japan cooperated with Russian and Chinese authorities in their mitigation efforts [1, 4-6, 15]. With no cure available, stopping transmission became the key aim of these efforts. Similar to the recent COVID-19 pandemic, these measures included isolation, quarantine, and “plague passports”. Those with suspected cases and those who had been in contact with infected people were quarantined on train carriages. They were released if no symptoms developed within five to ten days and given a wire wristband fastened with a lead seal declaring they were plague free [2, 4, 5]. In the case of deaths at home, the entire household was immediately isolated, and contaminated property was burned to prevent infection [1-2, 4-6, 14]. Sanitary zones were established, and police monitored the population.
A local Chinese-Malayan physician educated at Cambridge University, Wu Lien-Teh (Wu Liande) (1879-1960), received imperial permission to cremate patients’ dead bodies (Figure 3). Wu Lien-Teh also conducted post-mortem examinations on plague victims after human dissection was legalized by presidential mandate. He confirmed that the plague was pneumonic, not bubonic, as it was at first assumed. With no remedy against the disease, the only way to defeat it was through education. Thus, he recommended everyone wear face masks [1, 2, 5, 6, 12, 14].

Figure 3 - Dr. Wu-Lien Teh. Source: Library of Congress Prints and Photographs Division Washington, D.C. Reproduction Number: LC-DIG-ggbain-14227 (digital file from original negative).
The Mukden Conference and Eradication of the Epidemic
During the first decade of the 20th century, before establishment of the World Health Organization, disease response was up to individual nations. The Great Manchurian Plague served as a “sanitary awakening” [16]. Recognizing the need for a multinational medical response to outbreaks such as the plague, several countries participated in the Mukden Conference, the first international scientific congress held in China in April 1911 [5, 6, 11, 17, 18]. Participants included the United States of America, Great Britain, Germany, France, Italy, Mexico, Netherlands, Austria- Hungary, Russia, Japan, and China. Thirty-three official representatives attended (Figure 4). Professor Kitasato chaired part of the conference, and Wu Lien-Teh served as its presider [5, 6, 18]. Influential delegates included Dr. Richard Strong (1872-1948) from the United States, Dr. Daniil Zabolotny (1866-1929) from Russia, and Dr. Reginald Farrar (1861-1921) from Great Britain [6, 19].
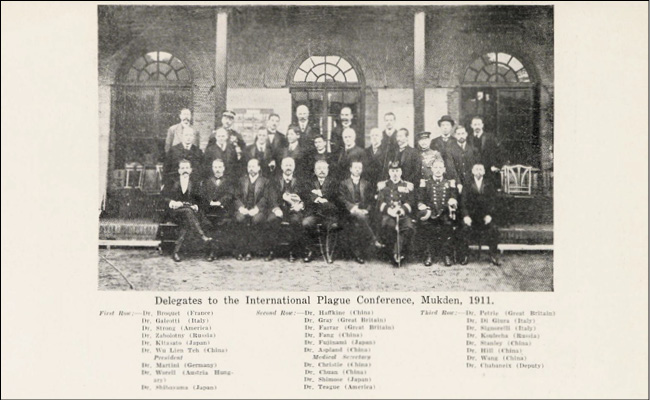
Figure 4 - Delegates to the International Plague Conference Mukden 1911. Source: Centre for Research in the Arts, Humanities and Social Sciences (CRASSH, The University of Cambridge).
Modes of contagion, as well as asymptomatic patients and super-spreaders, were among the main topics discussed. The Mukden Conference motivated the establishment of the North Manchurian Plague Prevention Service in 1912. For the first time, China was embracing a Western approach to medical care, with the intention of promoting public health during the first years of Chinese Republic (1912-1949) [1, 2, 5, 6, 11, 19].
In addition to the dire public health consequences, the plague outbreak in Manchuria devastated the Chinese economy, especially the fur and soybean trades, due to the port and railway closures [4, 20]. Still, these strict closures and protocols (e.g., quarantine, mask use) led to significant reductions in transmission in most regions of China. Closing of the Dalian port also prevented expansion of the disease to Japan, Korea, and Hong Kong [4, 5].
The last case of the Manchurian plague was recorded on March 1, 1911. Everything, including the South Manchurian Railway, reopened. As a result of Wu Lian-Teh’s drastic measures, the epidemic was declared over by the end of April 1911. The region returned to normal, and subsequent cases of the plague were successfully confined to hospitals [4, 5].
CONCLUSIONS
The Great Manchurian Plague occurred at a crucial moment and in a geopolitically important area. China, Russia, and Japan had imperial aspirations to dominate the region, but the disease outbreak forced them to work together. With a mortality rate near 100%, the outbreak claimed the lives of more than 60,000 people in the region. Despite or perhaps because of these dire public health consequences, the Manchurian plague served as an incentive for China to embrace new approaches to medical care. Similar to the COVID-19 pandemic, this widespread and deadly outbreak served as a reminder that swift and cooperative responses are critical approaches in addressing global public health issues.
Acknowledgments
We would like to thank Michaël Davy, Photo library manager-Institut Pasteur Centre de Ressources en Information Scientifique (CeRIS) for his kind assistance and the permission to reproduce the image from Institut Pasteur/Archives Henri Mollaret.
Conflict of interest
None to declare
Funding
None
REFERENCES
[1] Farrar R. Plague in Manchuria. Proc R Soc Med. 1912; 5 (Epidem_State_Med), 1-24. doi: 10.1177/003591571200501401.
[2] Rogaski R. The Manchurian Plague and COVID-19: China, the United States, and the “Sick Man”, Then and Now. Am J Pub Health. 2021; 111, 423-9. doi: 10.2105/AJPH.2020.305960.
[3] Lynteris Chr. Plague masks: the visual emergence of anti-epidemic personal protection equipment. Med Anthropol. 2018; 37 (6), 442-57. doi: 10.1080/01459740.2017.1423072.
[4] Summers W. The Great Manchurian Plague of 1910-1911. The Geopolitics of an Epidemic Disease. Yale University Press, New Haven & London, 2012.
[5] Gramsa M. The Epidemic of Pneumonic Plague in Manchuria 1910-1911. Past & Present. 2006; 190, 147-83.
[6] Chernin E. Richard Pearson Strong and the Manchurian Epidemic of Pneumonic Plague, 1910-1911. J Hist Med All Scis. 1989; 44 (3), 296-319. doi: 10.1093/jhmas/44.3.296.
[7] Sebbane F, Jarett C, Gardner D, Long D, Hinnebusch J. Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc Nat Acad Sci. 2006; 103 (14), 5526-30. doi: 10.1073/pnas.0509544103.
[8] Bockemühl J. 100 Jahre nach der Entdeckung der Pesterreger. Bedeutung und Verehrung von Alexandre Yersin in Vietnam heute. Immunität und Infektion. 1994; 22 (2), 72-5. PMID: 7959865.
[9] Howard-Jones N. Was Shibasaburo Kitasato the Co-Discoverer of the Plague Bacillus? Persp Biol Mede. 1973; 16 (2), 292-307. doi: 10.1353/pbm.1973.0034.
[10] World Health Organization. Plague. Available at: https://www.who.int/en/news-room/fact-sheets/detail/plague [accessed 8 June 2021].
[11] Teh WL, Han CW, Pollitzer R. Plague in Manchuria. Observations made during and after the second Manchurian plague epidemic in 1920-1921. The role of the tarabagan in the epidemiology of plague. J Hyg. 1923; 21 (3), 307-58. doi: 10.1017/s0022172400031521.
[12] Glatter KA, Finkelman P. History of the Plague: An Ancient Pandemic for the Age of COVID-19. Am J Med. 2021; 134 (2), 176-81. doi: 10.1016/j.amjmed.2020.08.019.
[13] Tsoucalas G, Michaleas SN, Papaioannou TG, Karamanou M. Covid-19 pandemic and Bats: a lucky symbol of evil fortune. Infez Med. 2021; 29 (2), 292-3.
[14] Teh WL, Han CW, Pollitzer R. Clinical Observations Upon the Manchurian Plague Epidemic, 1920-1921. J Hyg. 1923; 21 (3), 289-306. PMID: 20474781.
[15] Bu L. Public Health and The Modernization of China 1865-2015. Routledge, United Kingdom. 2020.
[16] Editorial. North Manchurian Plague Prevention Service. British Medical Journal. 1914; 1 (2790), 1360.
[17] Editorial. The International Plague Conference in Manchuria. Brit Med J. 1911; 1 (2627), 1063-4.
[18] Teh WL. Inaugural address delivered at the opening of the International Plague Conference, Mukden, April 4th 1911. Tientsin Press, Tianjin, 1911.
[19] Editorial. The International Plague Conference at Mukden. The Lancet. 1911; 177 (4577), 1382-3. doi: 10.1016/S0140-6736(01)62725-9.
[20] Li D, Li N. Moving to the Right Place at the Right Time: The Economic Consequence of the Manchuria Plague of 1910-11 on Migrants (October 31, 2013). Available at SSRN: https://ssrn.com/abstract=2351650. doi: 10.2139/ssrn.2351650.